Cancer survivors’ other medical problems poorly managed

People who survive cancer are less likely to receive necessary care for a wide range of other non-cancer-related medical problems according to a new study published September 13, 2004 in the online edition of CANCER, a peer-reviewed journal of the American Cancer Society. The study suggests that a history of cancer may cause health care providers to ignore other chronic medical ailments, such as heart disease, heart failure, diabetes, and lung disease. The abstract of this article will be freely accessible via the CANCER News Room.
Thanks in part to improved survival rates, the number of people in the U.S. with a history of cancer is well over 9.6 million and expected to rise. As cancer survivors grow older, not only do they have to be vigilant about monitoring for relapse, but they are also vulnerable to the same common chronic ailments that afflict aging Americans, such as diabetes, heart disease, strokes, and other cancers.
While previous studies have shown that cancer survivors have more contact with physicians, there is little evidence that this translates into adequate care for non-cancer-related health care diseases. In fact, studies show cancer survivors who see only their primary care doctor are less likely to receive even recommended cancer screening tests.
Craig C. Earle, M.D., M.Sc. and Bridget A. Neville, M.P.H. of the Dana-Farber Cancer Institute in Boston reviewed data from the Centers for Disease Control and Prevention’s Surveillance, Epidemiology, and End Results (SEER) program to compare Medicare claims from more than 14,000 colon-cancer survivors with a group of healthy controls.
The authors found colorectal cancer survivors were less likely than healthy controls to receive recommended medical care for the management of their chronic diseases. Significantly, outpatient medical conditions were undermanaged and consisted of a broad range of diseases, including stable angina, diabetes, and chronic lung disease. Cancer survivors were also less likely to receive recommended preventive care, such as immunizations or cholesterol screening.
Significantly, patients followed by both a primary care physician and an oncologist received the greatest proportion of recommended care while those only followed by an oncologist received the least recommended non-cancer care.
The authors say there is no good rationale for not providing cancer survivors with appropriate follow up care for many chronic conditions, and conclude their findings “raise the possibility that either a blinding focus on the prior malignancy or nihilism about the prognosis may leave cancer patients’ other medical issues relatively ignored.”
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Properties of new materials for microchips
… can now be measured well. Reseachers of Delft University of Technology demonstrated measuring performance properties of ultrathin silicon membranes. Making ever smaller and more powerful chips requires new ultrathin…

Floating solar’s potential
… to support sustainable development by addressing climate, water, and energy goals holistically. A new study published this week in Nature Energy raises the potential for floating solar photovoltaics (FPV)…
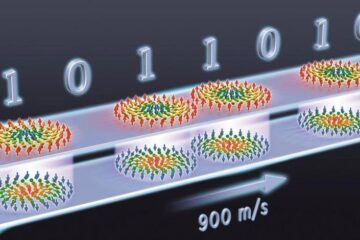
Skyrmions move at record speeds
… a step towards the computing of the future. An international research team led by scientists from the CNRS1 has discovered that the magnetic nanobubbles2 known as skyrmions can be…





















