Guidelines for food allergy testing

A blood test that measures food-specific allergy antibodies can be used to help pediatric allergists with the difficult decision of when to reintroduce a food that a child has been allergic to, say researchers at the Johns Hopkins Children’s Center.
In their report, published in the July issue of The Journal of Allergy and Clinical Immunology, the researchers provide guidelines for using these antibody levels to determine which children should be offered an additional allergy test, known as an oral food challenge, in which the child eats small amounts of the food allergen to establish whether or not a food allergy really exists.
Based on results of their investigation into how well IgE antibody levels could predict children’s reactions on the oral food challenge test, the Hopkins team specifically recommends that challenge tests for milk, egg, and peanut be performed on children with at least a 50-50 chance of “passing.”
This 50-50 challenge pass rate was most clear for milk, egg, and peanut and was associated with low levels (less than 2.0 kilounits of antibody per liter of blood) of food-specific IgE, the antibodies produced by the immune system that can cause allergic reaction. These antibodies can be measured using a test that is available in most commercial labs.
“These findings make it clear that doing a blood test to measure IgE levels can accurately predict how a patient will fare during a food challenge, and we recommend its routine use in clinical practice to screen children with suspected allergies before a food challenge is performed,” says Robert Wood, M.D., a pediatric allergist at the Johns Hopkins Children’s Center and the study’s senior author.
“By using our data as a guideline, physicians can better determine the appropriate time to try to reintroduce foods into an allergic child’s diet,” Wood adds. “An historical lack of such guidelines has led to considerable indecision in the appropriate timing of food challenges.”
Patients with IgE levels of 2.0 kilounits or less – who fall under the new Hopkins guidelines – are more likely to pass a food challenge because their low IgE levels could indicate a developed tolerance to the allergen or a previous allergy misdiagnosis. “Without a definitive allergy diagnosis from a food challenge, children with low IgE levels who may no longer be allergic, or who were misdiagnosed with a food allergy, may be unnecessarily avoiding foods like milk, eggs, and peanuts which have significant nutritional benefits,” Wood says.
On the flip side, when the expected pass rate for a food challenge is less than 50 percent, or for IgE levels of more than 2.0 kilounits, he says it’s very likely that the patient has a legitimate food allergy and therefore does not need his or her allergy confirmed through a food challenge, which could cause a significant allergic reaction.
In the study, researchers reviewed the charts of 391 children who underwent 604 oral food challenges to milk, egg, peanut, soy, and wheat at the Children’s Center from 1999-2001. They discovered that levels of IgE allergy antibodies against milk, egg, and peanut were significantly higher in those patients who had an allergic reaction and “failed” a food challenge compared to those who “passed.” Data for soy and wheat were less clear.
Although food challenges have long been the “gold standard” for diagnosing food allergies, Wood says physicians do not have any clear, clinical guidelines to help them determine when a food challenge should be considered, meaning it’s possible some children who could benefit from the test may be overlooked.
During a food challenge, patients are fed increasing doses of the suspected allergen while being monitored by a physician for symptoms of an allergic reaction, including hives, coughing, difficulty breathing and vomiting. Because of the possibility of a severe allergic reaction, oral food challenges must take place in a clinical setting while under a physician’s supervision.
Experts say food allergies are extremely common, affecting up to 8 percent of children and 2 percent of adolescents and adults. In young children, the foods most likely to cause allergies are cow’s milk, eggs, wheat and peanuts. In older children and adults, peanut and seafood allergies are most common. Other foods that commonly cause allergic reactions include soy products and tree nuts, such as almonds, pecans, and Brazil nuts.
Media Contact
More Information:
http://www.jhmi.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
Silicon Carbide Innovation Alliance to drive industrial-scale semiconductor work
Known for its ability to withstand extreme environments and high voltages, silicon carbide (SiC) is a semiconducting material made up of silicon and carbon atoms arranged into crystals that is…
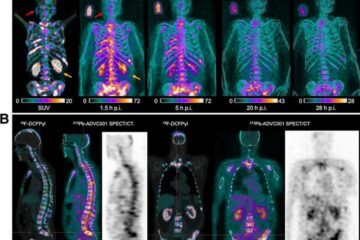
New SPECT/CT technique shows impressive biomarker identification
…offers increased access for prostate cancer patients. A novel SPECT/CT acquisition method can accurately detect radiopharmaceutical biodistribution in a convenient manner for prostate cancer patients, opening the door for more…

How 3D printers can give robots a soft touch
Soft skin coverings and touch sensors have emerged as a promising feature for robots that are both safer and more intuitive for human interaction, but they are expensive and difficult…





















