Researchers identify novel method of distinguishing Alzheimer’s disease from other types of dementia

Nearly a century after Alzheimer’s disease was first identified, there has been no foolproof way to diagnose the illness in a living patient. But a new method used by doctors at UT Southwestern Medical Center at Dallas is almost 100 percent accurate when combined with clinical assessment.
Testing blood flow in a specific region of the brain may boost the degree of diagnostic certainty in difficult cases from 90 percent to almost 100 percent, said Dr. Frederick Bonte, director of the Nuclear Medicine Center at UT Southwestern.
A study appearing today in the Journal of Nuclear Medicine shows that single-photon emission computed tomography (SPECT) can be used to identify a characteristic sign of Alzheimer’s disease and distinguish it from a group of illnesses known as frontotemporal diseases, which comprise the second-leading cause of dementia in the elderly.
SPECT is a radioisotope test that produces a three-dimensional picture of the amount of blood flowing in certain regions of the brain. People with Alzheimer’s have reduced blood flow in some areas of the brain, one of which is called the posterior cingulate cortex. This region helps process information from the parietal cortex and the hippocampus, which are responsible for storing vocabulary words and geographical information.
“This is the first publication using the posterior cingulate to rule out frontotemporal disease,” said Dr. Bonte, the study’s lead author. “If the blood flow is significantly reduced to that structure, you have identified Alzheimer’s, and you have simultaneously excluded the frontotemporal dementias.
“The dementing diseases are becoming a very important socio-economic problem, in addition to being a group of scientific problems of incredible difficulty. The prospects are quite hopeful now that effective treatments for Alzheimer’s disease – and possibly a cure – will emerge in the not-too-distant future. This makes it even more important to find out who really has Alzheimer’s disease and is, therefore, eligible for treatment and who has one of the other dementing diseases, for whom these new treatments would be ineffective.”
In the study, SPECT was used to measure brain blood flow in the posterior cingulate cortex of 60 people, aged 54 to 92. Twenty of the patients were suspected of having Alzheimer’s disease; 20 were suspected of having frontotemporal disease; and the remaining 20 were normal volunteers with no evidence of dementia.
Of those suspected of having Alzheimer’s, 16 exhibited significant blood-flow reductions in the posterior cingulate cortex. Of the 20 patients suspected of having frontotemoporal disease, only one showed signs of reduced blood flow in the region. That patient was later re-evaluated and diagnosed with Alzheimer’s disease.
Dr. Linda Hynan, a UT Southwestern biostatistician and assistant professor and co-author of the paper, said this study shows that patients with poor blood flow in the posterior cingulate cortex are 16 times more likely to have Alzheimer’s disease than one of the frontotemporal dementias.
Evidence of shrinkage in brain structures such as the hippocampus and parietal cortex is also central to diagnosing Alzheimer’s. This shrinkage, or atrophy, can be seen on a standard MRI. Still, autopsy remains the definitive diagnostic tool for Alzheimer’s disease.
Alzheimer’s disease affects 4 million Americans and accounts for 70 percent of dementia-causing diseases. Symptoms may include memory loss, personality changes, trouble finding words and feeling lost in familiar places. Ten percent to 15 percent of adults 65 or older in the United States have Alzheimer’s disease.
Dr. Bonte, who founded the medical center’s Department of Radiology in 1956, has been involved in research and clinical diagnosis of Alzheimer’s for 24 years.
UT Southwestern’s Alzheimer’s Disease Center is one of 29 such centers nationwide supported by the National Institute on Aging.
Other UT Southwestern authors included Thomas Harris, a senior research scientist in radiology, and Celeste Roney, a graduate student.
This study was funded by grants from the National Institutes of Health and Amersham Health.
To automatically receive news releases from UT Southwestern via e-mail, subscribe at http://www.utsouthwestern.edu/utsw/cda/dept37326/files/37813.html
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Combatting disruptive ‘noise’ in quantum communication
In a significant milestone for quantum communication technology, an experiment has demonstrated how networks can be leveraged to combat disruptive ‘noise’ in quantum communications. The international effort led by researchers…
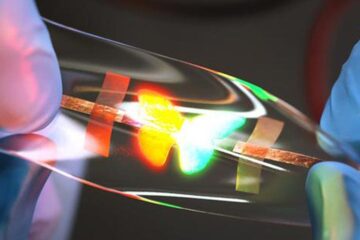
Stretchable quantum dot display
Intrinsically stretchable quantum dot-based light-emitting diodes achieved record-breaking performance. A team of South Korean scientists led by Professor KIM Dae-Hyeong of the Center for Nanoparticle Research within the Institute for…

Internet can achieve quantum speed with light saved as sound
Researchers at the University of Copenhagen’s Niels Bohr Institute have developed a new way to create quantum memory: A small drum can store data sent with light in its sonic…





















