Researchers find new way to trigger self-destruction of certain cancer cells

Discovery could lead to new drug therapy for some childhood cancers
Investigators at St. Jude Children’s Research Hospital have discovered a previously unrecognized way that certain types of cancer cells can be forced to activate a self-destruction program called apoptosis.
The finding suggests that drugs designed to activate apoptosis might be effective anti-cancer therapies. This strategy would target specific molecules in the cancer cell rather than rely on chemotherapy, which has serious side effects that degrade quality of life. The research is published in the June 20 issue of Molecular Cell.
The St. Jude team stimulated apoptosis by treating cancer cells with a drug called rapamycin, which blocks the action of a protein called mTOR. This protein stimulates a biochemical pathway that leads to increased production of proteins essential for cell proliferation. Blocking mTOR with rapamycin leaves the cell unable to make these critical proteins.
Blocking the activity of mTOR with rapamycin triggers a biochemical pathway called the JNK cascade in cells that lack a gene called p53, according to Peter Houghton, Ph.D., chair of the St. Jude Department of Molecular Pharmacology. Since p53 is mutated and inactive in about half of all types of cancer, blocking mTOR and activating apoptosis in cells with mutated p53 has potentially wide application. Houghton is senior author of the paper reporting these results.
“Shutting down synthesis of proteins essential for cell proliferation by blocking mTOR sends the cell into a crisis,” Houghton said. “The cell activates a protein called ASK1, which is at the top of the JNK cascade. ASK1 then sets off the JNK cascade and causes the cells that lack p53 to self-destruct.”
In cells that have a functional p53 gene, (e.g., normal cells), a protein called p21 is expressed and–in the presence of rapamycin–binds to ASK1 and inactivates it. This prevents the cell from undergoing apoptosis.
The investigators also found that the stress caused by rapamycin requires the presence of a protein called 4E-BP1. This protein stops the cell from using use some types of mRNA (the “decoded” form of DNA) to make proteins, including survival factors. 4E-BP1 is normally held in check by mTOR; so the cell continues to use mRNA to make proteins that are essential for proliferation. However, when rapamycin blocks mTOR, 4E-BP1 is free to put the brakes on.
In cells lacking p53, activation of the JNK cascade by rapamycin occurs so quickly that it might not be caused directly by the inhibition of protein synthesis.
“Right now, we don’t know exactly what sends the cell into crisis after rapamycin blocks mTOR,” Houghton said. “Further study is needed to determine what the link is between shutting down production of specific proteins and the cellular crisis that prompts cells to undergo apoptosis.”
The strategy of using rapamycin to block mTOR and activate ASK1 could be thwarted by another survival factor, called IGF-I.
“IGF-I prevents rapamycin from activating ASK1, and therefore shuts down the pathway that leads to apoptosis,” Houghton said. “So any drug therapy that targets mTOR with the intent of inducing cell death should also include a drug that targets IGF-I signaling. That double hit would leave the cancer cell no choice but to self-destruct.”
For this research, Houghton’s team used Rh30 cells–rhabdomyosarcoma cells lacking p53. The team showed that rapamycin caused sustained activation of the JNK cascade; and that exposure of Rh30 cells to IGF-I completed blocked the activation of c-Jun, a critical protein in the JNK cascade that is activated by rapamycin.
The team also showed that the Rh30 cells could be thrown into a crisis by starving them of amino acids, the building blocks of proteins. This stress required the presence of 4E-BP1 and activation of ASK1. Rh30 cells with rapamycin-resistant mTOR did not respond to the drug by triggering apoptosis. This was strong evidence that rapamycin had its effect on apoptosis by blocking mTOR.
St. Jude investigators are now planning clinical trials of two drugs that are rapamycin analogs (slight chemical modifications of rapamycin). The drugs, CCI779 (Wyeth-Ayerst) and RAD001 (Novartis), will be investigated for safety. Clinical trials will investigate their effectiveness in treating neuroblastoma, a cancer of specialized nerve cells involved in the development of the nervous system and other tissues.
Other authors of the paper include Shile Huang, Lili Shu, Michael B. Dilling, John Easton, Franklin C. Harwood (St. Jude) and Hidenori Ichijo (Tokyo Medical and Dental University; Tokyo, Japan).
Contact: Bonnie Cameron, bonnie.cameron@stjude.org
Media Contact
More Information:
http://www.stjude.orgAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
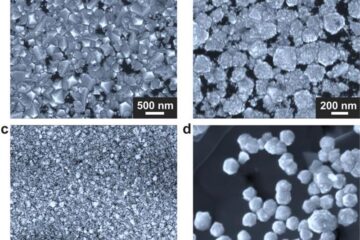
Making diamonds at ambient pressure
Scientists develop novel liquid metal alloy system to synthesize diamond under moderate conditions. Did you know that 99% of synthetic diamonds are currently produced using high-pressure and high-temperature (HPHT) methods?[2]…
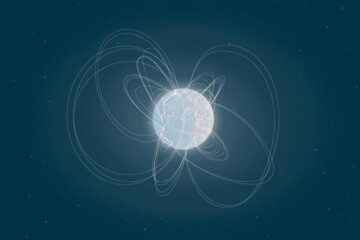
Eruption of mega-magnetic star lights up nearby galaxy
Thanks to ESA satellites, an international team including UNIGE researchers has detected a giant eruption coming from a magnetar, an extremely magnetic neutron star. While ESA’s satellite INTEGRAL was observing…
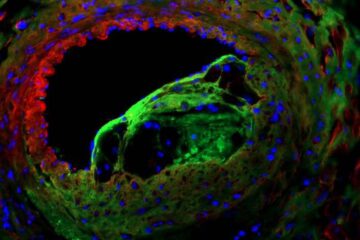
Solving the riddle of the sphingolipids in coronary artery disease
Weill Cornell Medicine investigators have uncovered a way to unleash in blood vessels the protective effects of a type of fat-related molecule known as a sphingolipid, suggesting a promising new…





















