Sleep disorder linked to common, serious heart rhythm problem

A heart rhythm disturbance that affects more than 2 million Americans is twice as likely to recur in patients with untreated sleep apnea, according to a Mayo Clinic study published in the May 27 edition of Circulation: Journal of the American Heart Association. Obstructive sleep apnea (OSA) is a condition that causes people to repeatedly stop breathing during sleep.
Atrial fibrillation (AF) is the most common sustained heart arrhythmia and can have serious consequences. When the upper chambers of the heart quiver rapidly and erratically — as many as 400 times per minute — blood does not move efficiently through the heart. This pooling blood is more likely to clot, leading to heart attacks or strokes. AF also can lead to heart failure by causing the heart’s main pumping chambers, the ventricles, to contract rapidly — often more than 100 beats per minute.
AF treatment involves using electrified paddles on the chest to shock the heart back into the proper rhythm, a procedure called cardioversion. Medications can help maintain normal rhythms, but lasting results are difficult to achieve; more than half of patients fall back into AF within one year.
In the Mayo Clinic study, OSA was the single factor most closely associated with recurrence of AF.
“Other recent studies have suggested that AF may be more common in patients with sleep apnea,” says Virend Somers, M.D., Ph.D., the Mayo Clinic cardiologist who led the study. “To our knowledge this is the first study showing that untreated OSA is associated with an increased risk of recurrent atrial fibrillation, and that the risk is not explained by other conditions but rather appears to be due to the presence of untreated OSA itself.”
Dr. Somers likens OSA to the collapse of a soda straw that has one end blocked. “In OSA, the upper part of the airway essentially collapses when people inhale during sleep. To overcome the obstruction, the patient breathes in harder, which generates very high negative pressures that can make the collapse worse,” he explains. “This raises blood pressure, lowers blood oxygen levels and stretches the walls of the atria, making them susceptible to irregular electrical rhythms.” One of several treatments for OSA is wearing a continuous positive airway pressure (CPAP) device while sleeping. CPAP uses tubes to apply air through the nose and mouth, which overcomes the collapse.
Dr. Somers’ group compared 43 AF patients who had been diagnosed with OSA with 79 controls who were also treated at the Mayo Clinic Cardioversion Center but had not been diagnosed with the sleep disorder. The researchers were able to follow 39 of the OSA patients, 27 of whom either got no OSA treatment or used it inappropriately (less than five times per week) for a year after cardioversion. AF recurred in 82 percent of the patients with untreated OSA, compared to 42 percent in the treated OSA group. The controls had a 53-percent recurrence rate.
The study results are particularly important because the prevalence of OSA increases with obesity, which is an American epidemic. “It is conceivable that a consequent increase in obstructive sleep apnea may contribute to the dramatic increase in the incidence of AF, which has nearly tripled during the past three decades,” Dr. Somers says.
“In the general population, the estimated prevalence of significant OSA is 24 percent for men and 9 percent for women ages 30 to 60, and is even higher when associated with obesity or cardiovascular disease, such as high blood pressure,” he explains. “Our control group had a high prevalence of obesity, so it is quite likely that many of those 79 control patients actually had undiagnosed — and therefore untreated — sleep apnea. Given the high prevalence of obstructive sleep apnea and the emerging epidemics of obesity and AF, our findings of an increased risk of AF in untreated OSA patients may have implications for both diseases.”
Dr. Somers suggests that selected patients with AF should be screened for OSA because successful treatment may reduce the risk for this heart rhythm disturbance. Leading candidates are those with recurrent AF who are obese, whose spouses say they snore loudly or who have seen them stop breathing, or who experience daytime sleepiness.
The lead author of the paper is Ravi Kanagala, M.D. Co-authors are Narayana Murali, M.D.; Paul Friedman, M.D.; Naser Ammash, M.D.; Bernard Gersh, M.B., Ch.B.; Karla Ballman, Ph.D.; and Abu Shamsuzzaman, M.D., Ph.D.
Media Contact
More Information:
http://www.mayo.edu/All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
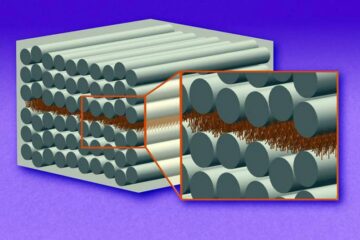
“Nanostitches” enable lighter and tougher composite materials
In research that may lead to next-generation airplanes and spacecraft, MIT engineers used carbon nanotubes to prevent cracking in multilayered composites. To save on fuel and reduce aircraft emissions, engineers…

Trash to treasure
Researchers turn metal waste into catalyst for hydrogen. Scientists have found a way to transform metal waste into a highly efficient catalyst to make hydrogen from water, a discovery that…
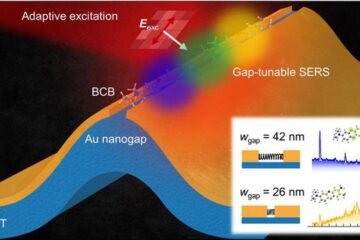
Real-time detection of infectious disease viruses
… by searching for molecular fingerprinting. A research team consisting of Professor Kyoung-Duck Park and Taeyoung Moon and Huitae Joo, PhD candidates, from the Department of Physics at Pohang University…





















