Energy blocker may be potential liver cancer treatment

A team of Johns Hopkins researchers has identified and successfully tested in animals a potential new treatment for liver cancer, a disease for which there are few effective treatments.
Writing in the July 15 issue of Cancer Research, the scientists report that only cancer cells were killed when the compound, 3-bromopyruvate, was given to rabbits with experimental liver tumors.
“It’s very exciting because we expected the compound to be pretty toxic, but somehow normal cells in the rabbit protect themselves against it,” says Peter Pedersen, Ph.D., professor of biological chemistry who has spent two decades studying energy production in cells and how it relates to cancer growth. “We even injected it into a vein so it was distributed throughout the rabbit, and we still didn’t see any apparent toxicity. It’s sort of amazing.”
A single injection of the compound directly into the artery that feeds the tumor killed a lot of the cancer cells, but left healthy liver alone. The researchers compared 3-bromopyruvate to a currently used treatment for human liver cancer, called chemoembolization, which delivers a dose of chemotherapy to the tumor and also blocks off the artery that feeds it.
“With 3-bromopyruvate in the rabbits, healthy liver seems to be spared, but sections of healthy liver were damaged by chemoembolization,” says first author Jeff Geschwind, M.D., associate professor of radiology and director of interventional radiology. “The difference was quite dramatic.”
Pedersen cautions that before 3-bromopyruvate could be tested in humans, scientists would need to learn how normal cells protect themselves, whether the compound causes long-term damage to normal tissues, and how increasing the dose affects the animals.
“We assume some level of the compound would be toxic,” adds Pedersen. “Any drug can be toxic, it’s a matter of determining the limits.”
Some 16,600 new cases of primary liver cancer are expected this year in the United States, but tumors that spread to the liver from elsewhere (so-called metastatic tumors) frequently hasten death from other, more prevalent types of cancer, such as skin, colon, breast and prostate cancers. If laboratory tests with other cancer cell types are promising, the compound might be useful for treating any tumor in the liver, not just ones originating there, the researchers say.
Two years ago, frustrated because most patients die within six months, Geschwind approached Pedersen with the idea of finding a new way to treat liver cancer. The plan: Identify potential new drugs and use intra-arterial delivery, a procedure with which Geschwind has considerable expertise, to get them directly into the tumor.
The timing was right, because Pedersen had learned enough about the role of energy production in liver cancer over the previous two decades to warrant looking for a possible new drug. Biological chemist Young Ko, Ph.D., now an assistant professor of radiology, tested a dozen or so possible energy-blocking molecules in the lab to find ones that could kill liver cancer cells.
In 2001, the team reported that already-available 3-bromopyruvate was head and shoulders above the rest, in part because it blocks both ways cells make energy (in the form of a molecule called ATP). “3-Bromopyruvate looks like a chemical found in our own body,” says Ko, who used 3-bromopyruvate in her graduate work years ago. “It shows a possible drug doesn’t have to be fancy or expensive; this is just as simple and as good as can be.”
Building on those laboratory studies, the researchers now have tested the compound’s effects in an animal model of liver cancer. Team member and pathologist Michael Torbenson, M.D., saw damage only to the tumor when he examined the tumor, liver, and other possibly affected organs from the rabbits. The researchers don’t understand how normal cells resist the compound’s effects, but cancer cells’ greater use of glucose to make energy may play a role.
In another experiment, the researchers discovered that small tumors in the lungs, buds from the original tumor in the liver, weren’t affected by arterial delivery of 3-bromopyruvate, but were substantially reduced by intravenous injection.
“It might be logical to treat tumors in the liver by direct intra-arterial injection, and then use an intravenous injection to kill cancer cells that have spread,” suggests Pedersen, “but knowing whether this is so is still a long way off.”
Media Contact
More Information:
http://cancerres.aacrjournals.org/All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

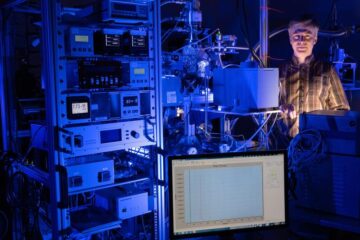
A flexible and efficient DC power converter for sustainable-energy microgrids
A new DC-DC power converter is superior to previous designs and paves the way for more efficient, reliable and sustainable energy storage and conversion solutions. The Kobe University development can…
Technical Trials for Easing the (Cosmological) Tension
A new study sorts through models attempting to solve one of the major challenges of contemporary cosmic science, the measurement of its expansion. Thanks to the dizzying growth of cosmic…
Peptides on Interstellar Ice
A research team led by Dr Serge Krasnokutski from the Astrophysics Laboratory at the Max Planck Institute for Astronomy at the University of Jena had already demonstrated that simple peptides…





















