Pre-Conception and Early Pregnancy Iron Deficiency Harms Brain

A mother’s iron deficiency early in pregnancy may have a profound and long-lasting effect on the brain development of the child, even if the lack of iron is not enough to cause severe anemia, according to a University of Rochester Medical Center study published in the scientific journal PLoS One.
The results are important because obstetricians might not notice or treat mild or moderate iron deficiency, and therefore the study authors believe their research underscores the need for monitoring a pregnant woman’s iron status beyond anemia.
Low iron is so common that an estimated 35 percent to 58 percent of all healthy women show some degree of deficiency. And among women of childbearing age, one in five has iron-deficient anemia, a more serious condition, according to the National Institutes of Health.
It is well established that iron-deficient babies develop more slowly and show brain abnormalities such as slow language learning and behavioral problems. But until now investigators did not know the degree to which iron deficiency in pregnancy is associated with these impairments, and when during gestation the deficiency has the most impact on the central nervous system.
“What convinced us to conduct the present study were our preliminary data suggesting that cells involved in building the embryonic brain during the first trimester were most sensitive to low iron levels,” said Margot Mayer-Proschel, Ph.D., the lead researcher and an associate professor of Biomedical Genetics at URMC.
Investigators, therefore, sought more details using a highly controlled animal model system, as it would not be feasible to study iron concentrations in developing human embryos. They found that the critical period begins in the weeks prior to conception and extends through the first trimester to the onset of the second trimester. Iron deficiency that starts in the third trimester did not seem to harm the developing brain.
“This information is very important for clinical care,” said Monique Ho, M.D., a collaborator on the study and assistant professor of Obstetrics and Gynecology and Pediatrics at URMC. “Prenatal care usually involves the recommendation of a multivitamin that contains iron, which is usually prescribed after pregnancy is confirmed or at the first prenatal visit. But not all women have access to prenatal care, and not all women can take the supplements in early pregnancy due to vomiting. This study suggests it might be prudent to begin routine monitoring to detect iron deficiency earlier.”
By studying the relationship between maternal iron intake and fetal iron levels through a diet study, the team was able to pin down the critical periods of gestation when the developing central nervous system was most vulnerable. They measured the resulting brain function using a common, non-invasive test called an auditory brainstem response analysis, or ABR.
Co-author Anne Luebke, Ph.D., an associate professor of Biomedical Engineering and Neurobiology & Anatomy at UR, suggested and directed the use of ABR testing, which can detect the speed of information moving from the ear to the brain. Investigators hoped to learn about impairments or changes in myelin, the insulating material that surrounds axons and is required for normal brain function.
“In addition, ABR testing is routinely performed on human infants, and thus our study has an important component that can be translated to a clinical setting,” Luebke said.
The most surprising aspect of the research, Mayer-Proschel said, was that the timing of the iron deficiency was much more important than the degree of deficiency. This observation also seems to argue against the common notion that the placenta can minimize the impact of the mother’s deficiency on the baby.
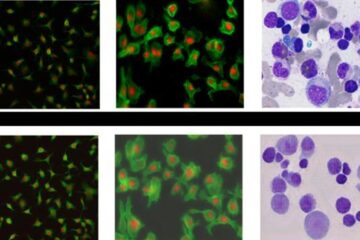
“We refer to this as the window of vulnerability,” she said, “and it seems to be at a very early stage of development.” In previous studies of the cellular targets of iron deficiency, Mayer-Proschel found that lack of iron sets off an imbalance of neural precursor cells, which might ultimately be responsible for the defects sometimes experienced by children up to age two.
“The next goals will be to better understand how maternal iron deficiency causes these changes in the offspring,” she said, “and most importantly, what are the opportunities for reversing the damage.”
The National Institutes of Health and the University of Rochester funded the research.
For Media Inquiries:
Leslie Orr
(585) 275-5774
Email Leslie Orr
Media Contact
More Information:
http://www.urmc.rochester.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Bringing bio-inspired robots to life
Nebraska researcher Eric Markvicka gets NSF CAREER Award to pursue manufacture of novel materials for soft robotics and stretchable electronics. Engineers are increasingly eager to develop robots that mimic the…

Bella moths use poison to attract mates
Scientists are closer to finding out how. Pyrrolizidine alkaloids are as bitter and toxic as they are hard to pronounce. They’re produced by several different types of plants and are…
AI tool creates ‘synthetic’ images of cells
…for enhanced microscopy analysis. Observing individual cells through microscopes can reveal a range of important cell biological phenomena that frequently play a role in human diseases, but the process of…





















