Pinpointing molecular path that makes antidepressants act quicker in mouse model
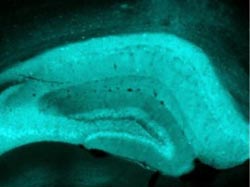
This is a mouse hippocampus expressing the Cre- virus. Credit: Julie Blendy, Ph.D.; Brigitta Gunderson, Ph.D.; Perelman School of Medicine, University of Pennsylvania<br>
The reasons behind why it often takes people several weeks to feel the effect of newly prescribed antidepressants remains somewhat of a mystery – and likely, a frustration to both patients and physicians.
Julie Blendy, PhD, professor of Pharmacology, at the Perelman School of Medicine, University of Pennsylvania; Brigitta Gunderson, PhD, a former postdoctoral fellow in the Blendy lab, and colleagues, have been working to find out why and if there is anything that can be done to shorten the time in which antidepressants kick in.
“Our goal is to find ways for antidepressants to work faster,” says Blendy.
The proteins CREB and CREM are both transcription factors, which bind to specific DNA sequences to control the “reading” of genetic information from DNA to messenger RNA (mRNA). Both CREB and CREM bind to the same 8-base-pair DNA sequence in the cell nucleus. But, the comparative influence of CREM versus CREB on the action of antidepressants is a “big unknown,” says Blendy.
CREB, and CREM to some degree, has been implicated in the pathophysiology of depression, as well as in the efficacy of antidepressants. However, whenever CREB is deleted, CREM is upregulated, further complicating the story.
Therefore, how an antidepressant works on the biochemistry and behavior in a mouse in which the CREB protein is deleted only in the hippocampus versus a wild type mouse in which CREM is overexpressed let the researchers tease out the relative influence of CREB and CREM on the pharmacology of an antidepressant. They saw the same results in each type of mouse line – increased nerve-cell generation in the hippocampus and a quicker response to the antidepressant. Their findings appear in the Journal of Neuroscience.
“This is the first demonstration of CREM within the brain playing a role in behavior, and specifically in behavioral outcomes, following antidepressant treatment,” says Blendy.
A Flood of Neurotransmitters
Antidepressants like SSRIs, NRIs, and older tricyclic drugs work by causing an immediate flood of neurotransmitters like serotonin, norepinephrine, and in some cases dopamine, into the synaptic space. However, it can take three to four weeks for patients to feel changes in mental state. Long-term behavioral effects of the drugs may take longer to manifest themselves, because of the need to activate CREB downstream targets such as BDNF and trkB, or as of yet unidentified targets, which could also be developed as new antidepressant drug targets.
The Penn team compared the behavior of the control, wild-type mice to the CREB mutant mice using a test in which the mouse is trained to eat a treat – Reese's Pieces, to be exact – in the comfort of their home cage. The treat-loving mice are then placed in a new cage to make them anxious. They are given the treat again, and the time it takes for the mouse to approach the treat is recorded.
Animals that receive no drug treatment take a long time to venture out into the anxious environment to retrieve the treat, however, if given an antidepressant drug for at least three weeks, the time it takes a mouse to get the treat decreases significantly, from about 400 seconds to 100 seconds. In mice in which CREB is deleted or in mice in which CREM is upregulated, this reduction happens in one to two days versus the three weeks seen in wild-type mice.
The accelerated time to approach the treat in mice on the medication was accompanied by an increase in new nerve growth in the hippocampus.
“Our results suggest that activation of CREM may provide a means to accelerate the therapeutic efficacy of current antidepressant treatment,” says Blendy. Upregulation of CREM observed after CREB deletion, appears to functionally compensate for CREB loss at a behavioral level and leads to maintained or increased expression of some CREB target genes. The researchers' next step is to identify any unique CREM target genes in brain areas such as the hippocampus, which may lead to the development of faster-acting antidepressants
Lisa A. Briand and Jennifer L. Onksen from the Department of Pharmacology, and John LeLay and Klaus H. Kaestner, from the Department of Genetics, were coauthors.
This work was supported by National Institute of Mental Health (U01MH0723832, T32-MH14654) and the National Cooperative Drug Discovery Group for the Treatment of Mood Disorders.
Penn Medicine is one of the world's leading academic medical centers, dedicated to the related missions of medical education, biomedical research, and excellence in patient care. Penn Medicine consists of the Raymond and Ruth Perelman School of Medicine at the University of Pennsylvania (founded in 1765 as the nation's first medical school) and the University of Pennsylvania Health System, which together form a $4.3 billion enterprise.
The Perelman School of Medicine has been ranked among the top five medical schools in the United States for the past 16 years, according to U.S. News & World Report's survey of research-oriented medical schools. The School is consistently among the nation's top recipients of funding from the National Institutes of Health, with $398 million awarded in the 2012 fiscal year.
The University of Pennsylvania Health System's patient care facilities include: The Hospital of the University of Pennsylvania — recognized as one of the nation's top “Honor Roll” hospitals by U.S. News & World Report; Penn Presbyterian Medical Center; and Pennsylvania Hospital — the nation's first hospital, founded in 1751. Penn Medicine also includes additional patient care facilities and services throughout the Philadelphia region.
Penn Medicine is committed to improving lives and health through a variety of community-based programs and activities. In fiscal year 2012, Penn Medicine provided $827 million to benefit our community.
Media Contact
More Information:
http://www.uphs.upenn.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Silicon Carbide Innovation Alliance to drive industrial-scale semiconductor work
Known for its ability to withstand extreme environments and high voltages, silicon carbide (SiC) is a semiconducting material made up of silicon and carbon atoms arranged into crystals that is…

New SPECT/CT technique shows impressive biomarker identification
…offers increased access for prostate cancer patients. A novel SPECT/CT acquisition method can accurately detect radiopharmaceutical biodistribution in a convenient manner for prostate cancer patients, opening the door for more…

How 3D printers can give robots a soft touch
Soft skin coverings and touch sensors have emerged as a promising feature for robots that are both safer and more intuitive for human interaction, but they are expensive and difficult…





















