Penn researchers repair immune system in leukemia patients following chemotherapy

A new treatment using leukemia patients' own infection-fighting cells appears to protect them from infections and cancer recurrence following treatment with fludarabine-based chemotherapy, according to new research from the Perelman School of Medicine at the University of Pennsylvania.
The new process is a step toward eliminating the harsh side effects that result from the commonly prescribed drug, which improves progression-free survival in patients with chronic lymphocytic leukemia (CLL) but destroys patients' healthy immune cells in the process, leaving them vulnerable to serious viral and bacterial infections. The drug's effects on the immune system tend to be so violent that it has been dubbed “AIDS in a bottle.”
Today at the 53rd American Society of Hematology Annual Meeting, the research team will present results showing how they use a patient's own T cells to repair his or her immune system after fludarabine treatment. With a restored immune system, patients can stop taking prophylactic antibiotics and may have prolonged progression-free survival.
“Fludarabine is a double-edged sword,” says Stephen J. Schuster, MD, an associate professor in the division of Hematology-Oncology and director of the Lymphoma Program at Penn's Abramson Cancer Center. “Although it is very active at killing CLL cells, it is also very active at killing normal cells in the immune system, particularly T lymphocytes, which are the master regulators of the immune system. So you rid the patient of their disease, but you also rid them of a normal immune system.”
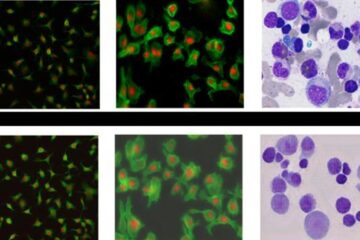
Thirty-four patients enrolled in the multicenter study. Prior to chemotherapy treatment, the researchers isolated healthy T lymphocytes from each patient's blood. When the patient finished chemotherapy, the team grew the T cells in Penn's Clinical Cell and Vaccine Production Facility using a technique that induces them to proliferate rapidly. The researchers then infused the expanded T cells back into the patient. “What we showed was that by giving them back their own T cells after treatment, we can restore patients' immune systems,” Schuster said.
“Within four weeks of the T cell infusion, their T cell counts were within the normal range.”
After chemotherapy and prior to T cell infusion, the median CD4 T cell count for fludarabine-treated patients was 119 cells/ml blood and the median CD8 T cell count was 80 cells/ml. Thirty days after the patients received the infusion of their own T cells, the median cell counts were in the normal range, at 373 cells/ml and 208 cells/ml for CD4 and CD8 cells, respectively. The T cell numbers remained in the normal range beyond 90 days, leading Schuster and colleagues to conclude that the autologous T cell transfer repaired the immune system of patients.
Although all of the patients' T cell counts returned to the normal range after treatment, not all patients responded equally well to the T cell therapy. Patients who had a complete response to chemotherapy had a more robust T cell recovery than did patients who had only a partial response. “We believe that having a complete remission of CLL seems to create a larger space for the normal immune cells to expand into,” Schuster says. “Somehow, the cancer seems to interfere with recovery of the immune system.”
In addition to quashing the complications ordinarily associated with treatment, the team hopes that the restored immune system will help keep the cancer in check. At a median follow-up of 14 months after T cell infusion, two-thirds of the patients remain progression-free. Longer follow up will be needed to compare treatment results for patients receiving T cells with published results for patients receiving similar chemotherapy without T cell support.
What is clear from the small trial is that patients can safely stop prophylactic antibiotic therapy after their T cell numbers rebound. Physicians regularly keep CLL patients on extended prophylactic antibiotic therapy to help stave off infections. In this study, though, patients stopped taking antibiotics about a month after receiving T cells without developing significant infections.
In addition to the Penn researchers, investigators from the MD Anderson Cancer Center, the Baylor College of Medicine, Texas Children's Hospital, and the Methodist Hospital in Houston also participated in the study.
The study was funded by the CLL Global Research Foundation.
This research will be presented Sunday, December 11, 2011 between 6 PM and 8 PM in Hall GH of the San Diego Convention Center.
Penn Medicine is one of the world's leading academic medical centers, dedicated to the related missions of medical education, biomedical research, and excellence in patient care. Penn Medicine consists of the Raymond and Ruth Perelman School of Medicine at the University of Pennsylvania (founded in 1765 as the nation's first medical school) and the University of Pennsylvania Health System, which together form a $4 billion enterprise.
Penn's Perelman School of Medicine is currently ranked #2 in U.S. News & World Report's survey of research-oriented medical schools and among the top 10 schools for primary care. The School is consistently among the nation's top recipients of funding from the National Institutes of Health, with $507.6 million awarded in the 2010 fiscal year.
The University of Pennsylvania Health System's patient care facilities include: The Hospital of the University of Pennsylvania — recognized as one of the nation's top 10 hospitals by U.S. News & World Report; Penn Presbyterian Medical Center; and Pennsylvania Hospital – the nation's first hospital, founded in 1751. Penn Medicine also includes additional patient care facilities and services throughout the Philadelphia region.
Penn Medicine is committed to improving lives and health through a variety of community-based programs and activities. In fiscal year 2010, Penn Medicine provided $788 million to benefit our community.
Media Contact
More Information:
http://www.uphs.upenn.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Bringing bio-inspired robots to life
Nebraska researcher Eric Markvicka gets NSF CAREER Award to pursue manufacture of novel materials for soft robotics and stretchable electronics. Engineers are increasingly eager to develop robots that mimic the…

Bella moths use poison to attract mates
Scientists are closer to finding out how. Pyrrolizidine alkaloids are as bitter and toxic as they are hard to pronounce. They’re produced by several different types of plants and are…
AI tool creates ‘synthetic’ images of cells
…for enhanced microscopy analysis. Observing individual cells through microscopes can reveal a range of important cell biological phenomena that frequently play a role in human diseases, but the process of…





















