Carnegie Mellon develops non-invasive technique to detect transplant rejection at cellular level

Research could revolutionize care of transplant patients
Carnegie Mellon University scientist Chien Ho and his colleagues have developed a promising tool that uses magnetic resonance imaging (MRI) to track immune cells as they infiltrate a transplanted heart in the early stages of organ rejection. This pre-clinical advance, described in an upcoming issue of the Proceedings of the National Academy of Sciences (PNAS), ultimately could provide a non-invasive way to detect transplant rejection in patients.
"We have reported for the first time the ability to monitor single immune cells in a live animal using MRI. This could revolutionize the management of transplant patients," said Ho, professor of biological sciences at the Mellon College of Science.
"Successful translation of this work to the clinic ultimately will reduce the number of biopsy procedures and should greatly improve the quality of life for cardiac transplant patients, especially children," added Ho, who directs the Pittsburgh NMR Center for Biomedical Research. "Perhaps most importantly, this advance will allow doctors to provide highly personalized care that could prevent transplant rejection."
Organ transplantation is the preferred clinical approach to treat end-stage organ failure, but transplant patients face a lifetime of immunosuppressive therapy and the risk of losing the new organ due to rejection. Physicians typically monitor patients for organ rejection following a heart transplant by performing frequent heart biopsies for the first year. Heart biopsies are invasive procedures that involve threading a catheter through the jugular vein to the heart’s right ventricle and snipping out several tiny pieces of tissue. A pathologist then tests the tissue to identify the presence of immune cells (such as macrophages) as well as other pathological changes in the transplanted heart tissue that indicate the graft is being rejected by the body’s immune system.
These procedures are costly, uncomfortable and must be repeated annually for a few years to monitor and treat any rejection. Biopsies also are problematic, according to Ho, because they do not look at the whole organ. By only sampling several small areas, a biopsy may miss the area of the transplanted organ where immune cells are gathering — one of the first signs of rejection.
Ho’s novel approach investigates transplant rejection non-invasively by observing macrophage accumulation in heart tissues using MRI.
"We were able to use MRI to visualize individual macrophages. By tracking individual cells, we also were able to observe, for the first time, that rejection progresses from the outside of the heart to the inside," said Ho. "Up to now, this phenomenon hasn’t been observed in pre-clinical or clinical research because biopsy samples are very limited in location and size."
The reported findings also have broader implications for biology and medicine, according to Ho.
"We now have the ability to visualize non-invasively and with sensitivity individual cells and their movement to targeted sites. Our new approach offers almost unlimited potential for monitoring cell therapies, such as those using stem cells, and for tracking cellular and developmental processes," Ho said.
For the research reported in PNAS, Yijen Wu, research biologist at the Pittsburgh NMR Center for Biomedical Research, tagged macrophages with nanometer (USPIO)- or micrometer (MPIO)-sized paramagnetic iron oxide particles, which are very sensitive to the magnetic fields used during MRI. Wu injected the MPIO or USPIO particles into rats that had received heart transplants three days earlier. Macrophages, which typically ingest foreign materials inside the body (bacteria, for example), incorporated the particles. Using MRI, the researchers then track tagged macrophages that infiltrate transplanted hearts. The locations of the tagged macrophages are highly defined and appear circular in shape, said Wu. This finding indicates that the new, real-time tracking method is very good at pinpointing exactly when and where rejection is taking place.
The researchers used a heterotropic heart model to study organ rejection. In this model, a rat receives a second functional heart, which is grafted into its abdomen. The rat’s native heart functions normally. In this way, the researchers can study how a transplanted heart changes through sequential stages of rejection while the rat stays healthy. This aspect of the research was conducted primarily by Qing Ye, a research biologist at the Pittsburgh NMR Center for Biomedical Research.
Ho’s team at the Pittsburgh NMR Center for Biomedical Research is now pursuing research using larger animal models. They are collaborating with researchers at the University of Pittsburgh School of Medicine, including Dr. David Cooper, professor of surgery in the Thomas E. Starzl Transplantation Institute; Dr. Jeffrey Teuteberg, assistant professor of medicine at the Cardiovascular Institute, Heart Failure/Transplantation; and Dr. Fernando Boada, associate professor in the Department of Radiology.
Media Contact
More Information:
http://www.andrew.cmu.eduAll latest news from the category: Medical Engineering
The development of medical equipment, products and technical procedures is characterized by high research and development costs in a variety of fields related to the study of human medicine.
innovations-report provides informative and stimulating reports and articles on topics ranging from imaging processes, cell and tissue techniques, optical techniques, implants, orthopedic aids, clinical and medical office equipment, dialysis systems and x-ray/radiation monitoring devices to endoscopy, ultrasound, surgical techniques, and dental materials.
Newest articles

Superradiant atoms could push the boundaries of how precisely time can be measured
Superradiant atoms can help us measure time more precisely than ever. In a new study, researchers from the University of Copenhagen present a new method for measuring the time interval,…
Ion thermoelectric conversion devices for near room temperature
The electrode sheet of the thermoelectric device consists of ionic hydrogel, which is sandwiched between the electrodes to form, and the Prussian blue on the electrode undergoes a redox reaction…
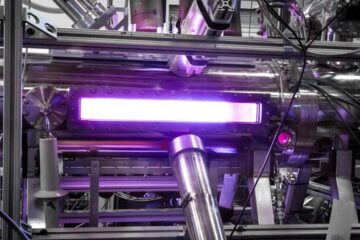
Zap Energy achieves 37-million-degree temperatures in a compact device
New publication reports record electron temperatures for a small-scale, sheared-flow-stabilized Z-pinch fusion device. In the nine decades since humans first produced fusion reactions, only a few fusion technologies have demonstrated…





















