Stem cells move one step closer to cure for genetic diseases
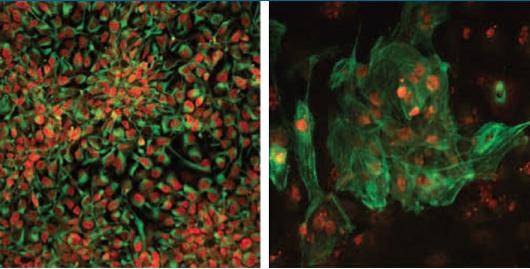
Salk researchers have generated disease-free stem cells from patients with mitochondrial disease that can be converted into any cell type including neuronal progenitors (left) or heart cells (right). These could potentially be used for future transplantation into patients. Credit: Salk Institute
“Right now, there are no cures for mitochondrial diseases,” says senior author Juan Carlos Izpisua Belmonte, professor in Salk's Gene Expression Laboratory. “Very recently, we've developed ways to prevent these diseases, so it was natural to next ask how we could treat them.”
Mitochondrial diseases are caused by any of about 200 mutations that affect the genes of mitochondria, tiny powerhouses inside nearly every cell of the body. Depending on the affected genes and cell types, the diseases can cause muscle weakness, liver disease, diabetes, seizures, developmental delays or vision problems. Existing therapies aim to ease the symptoms or slow the progression of the diseases, but can't entirely cure them.
In their new work, Belmonte and collaborators from around the world collected skin samples from patients with mitochondrial encephalomyopathy or Leigh Syndrome, both severe disorders that affect the brain and muscles.
The teams began by using current standard protocols to derive pluripotent stem cells from the skin cells, a process that resets the cells to their most basic state.
“During the process of stem cell generation, you spontaneously get different types of clones,” says Alejandro Ocampo, a research associate in Izpisua Belmonte's lab and one of the authors of the new paper. If the patient cells have an initial mix of healthy and diseased mitochondria, healthy and diseased stem cells will be generated. Then, the stem cells with healthy mitochondria can be picked out.
For some patients, though, this straightforward approach doesn't work; their cells don't have enough–or any–healthy mitochondria to start with.
So the team came up with a second approach: move the nucleus of the patient's skin cells, which contains most of their genes, into a donor egg cell with healthy mitochondria. Then, use the new egg cell to generate pluripotent stem cells. When the researchers did this, they found the healthy mitochondria took over, and healthy, genetically similar cells from the patient were successfully generated.
“In either case, the idea is that we have healthy stem cells, and we know how to convert pluripotent stem cells into different cell types,” says Jun Wu, an author of the paper and research associate in Izpisua Belmonte's lab. “They have the potential to give rise to every cell type in the body.”
For now, that means that researchers can use the healthy cells to generate heart, brain, muscle or eye cells from the mutation-free stem cells. But methods to make those cells fully mature and functional and transplant them into patients are still under development.
The new method will also be a boon to basic research, Izpisua Belmonte adds. Scientists have long struggled to understand why different organs and tissues are affected so differently by mitochondrial mutations. By comparing stem cells with mitochondrial mutations with healthy ones, and coaxing each to develop into different cell types, they can study this aspect of mitochondrial diseases in more detail.
###
Other researchers on the study were Li Ma of the Salk Institute; Hong Ma, Riffat Ahmed, Eunju Kang, Yeonmi Lee, Tomonari Hayama, Ying Li Crystal Van Dyken, Nuria Marti Gutierrez, Rebecca Tippner-Hedges, Amy Koski, Nargiz Mitalipov, Paula Amato, Don P. Wolf, and Shoukhrat Mitalipov of Oregon Health & Science University; Clifford D. L. Folmes, and Andre Terzic of the Mayo Clinic; Robert Morey, Sergio Mora-Castilla, and Louise C. Laurent of the University of California, San Diego; Joanna Poulton of the University of Oxford; and Xinjian Wang and Taosheng Huang of Cincinnati Children's Hospital.
The work was supported by the G. Harold and Leila Y. Mathers Charitable Foundation and the Leona M. and Harry B. Helmsley Charitable Trust.
About the Salk Institute for Biological Studies:
The Salk Institute for Biological Studies is one of the world's preeminent basic research institutions, where internationally renowned faculty probes fundamental life science questions in a unique, collaborative and creative environment. Focused both on discovery and on mentoring future generations of researchers, Salk scientists make groundbreaking contributions to our understanding of cancer, aging, Alzheimer's, diabetes and infectious diseases by studying neuroscience, genetics, cell and plant biology, and related disciplines. Faculty achievements have been recognized with numerous honors, including Nobel Prizes and memberships in the National Academy of Sciences. Founded in 1960 by polio vaccine pioneer Jonas Salk, MD, the Institute is an independent nonprofit organization and architectural landmark.
Media Contact
All latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles

High-energy-density aqueous battery based on halogen multi-electron transfer
Traditional non-aqueous lithium-ion batteries have a high energy density, but their safety is compromised due to the flammable organic electrolytes they utilize. Aqueous batteries use water as the solvent for…

First-ever combined heart pump and pig kidney transplant
…gives new hope to patient with terminal illness. Surgeons at NYU Langone Health performed the first-ever combined mechanical heart pump and gene-edited pig kidney transplant surgery in a 54-year-old woman…

Biophysics: Testing how well biomarkers work
LMU researchers have developed a method to determine how reliably target proteins can be labeled using super-resolution fluorescence microscopy. Modern microscopy techniques make it possible to examine the inner workings…





















