Gene therapy for muscular dystrophy fixes frail muscle cells in animal model

A new gene therapy technique that has shown promise in skin disease and hemophilia might one day be useful for treating muscular dystrophy, according to a new study by researchers at Stanford University School of Medicine.
In the study, scheduled to be published online in the Proceedings of the National Academy of Sciences the week of Jan. 2, the researchers used gene therapy to introduce a healthy copy of the gene dystrophin into mice with a condition that mimics muscular dystrophy. The dystrophin gene is mutated and as a result produces a defective protein in the roughly 20,000 people in the United States with the most common form of the disease.
Using gene therapy to treat muscular dystrophy isn’t a new idea. Thomas Rando, MD, PhD, associate professor of neurology and neurological sciences, said that researchers have tried several different techniques with variable success. One hurdle is getting genes into muscle cells all over the body. Another is convincing those cells to permanently produce the therapeutic protein made by those genes.
The gene therapy technique Rando and postdoctoral fellow Carmen Bertoni, PhD, used was developed by Michele Calos, PhD, associate professor of genetics. One of the main advantages of this method is that it could potentially provide a long-term fix for a variety of genetic diseases, including muscular dystrophy.
In muscular dystrophy, the muscle cells break down and are slowly replaced by fat. Eventually people with the disease are confined to a wheelchair and usually die in their 20s. There is currently no effective treatment for the disease, which explains why gene therapy remains a hope despite the significant hurdles.
Rando said the PNAS paper highlights an additional requirement for any gene therapy to be successful: the introduced gene must produce healthy dystrophin protein in large quantities in order to repair the entire muscle cell. Previous muscular dystrophy gene therapy studies did not look at whether the introduced dystrophin spread along the entire length of the muscle cell, which can be many millimeters long in mice or inches long in humans.
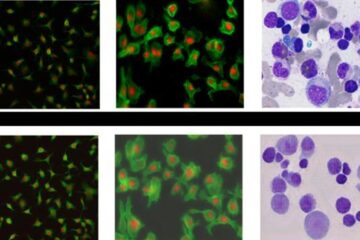
In the upcoming paper Bertoni used a standard gene therapy method to introduce two genes – dystrophin and a gene that makes a glowing protein – into mice with a mouse version of muscular dystrophy. She found that in mice producing insufficient dystrophin, she could see the glowing protein slowly leak out of the cell. This leakiness is a sign that the cell is not healed. In contrast, when she used Calos’ gene therapy technique to introduce the genes, the muscle cell contained high levels of dystrophin distributed along the length of the cell and the glowing protein stayed within the cell, suggesting that the abundant dystrophin repaired the ailing muscle.
“If you have a single cell that’s a foot long and you only correct a few inches, you’ve done very little,” Rando said, “Whereas if you correct it from end to end, you truly cure the disease in that cell.”
Both Rando and Calos point out that the road to a gene therapy cure for muscular dystrophy is still a long one. However, Calos is confident that her technique will be a part of the journey towards a cure for the disease and for other diseases such as hemophilia and the skin disease, epidermolysis bullosa. Early trials using her approach have looked promising in animal models of both of these diseases.
“I think our approach has a lot of potential to overcome issues that have slowed the field of gene therapy,” Calos said.
Calos said her approach has two advantages: one is that in her method the gene gets inserted directly into the cell’s own DNA, which is why the correction is permanent. In some other methods the gene stays outside the DNA and slowly breaks down. The second advantage is that her method doesn’t rely on a virus to disperse the DNA and therefore avoids some of the issues, including cancer and an immune reaction, that have turned up in viral gene therapy trials. Instead this approach uses naked DNA that travels through the bloodstream to cells of the body.
For his part, Rando said that no matter how well gene therapy works in an isolated muscle, researchers still must figure out how to get that gene to muscles throughout the body. Despite the remaining hurdles, both Rando and Calos said that their study is a step towards eventually treating muscular dystrophy and other diseases using gene therapy.
Media Contact
More Information:
http://www.stanford.eduAll latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles

Bringing bio-inspired robots to life
Nebraska researcher Eric Markvicka gets NSF CAREER Award to pursue manufacture of novel materials for soft robotics and stretchable electronics. Engineers are increasingly eager to develop robots that mimic the…

Bella moths use poison to attract mates
Scientists are closer to finding out how. Pyrrolizidine alkaloids are as bitter and toxic as they are hard to pronounce. They’re produced by several different types of plants and are…
AI tool creates ‘synthetic’ images of cells
…for enhanced microscopy analysis. Observing individual cells through microscopes can reveal a range of important cell biological phenomena that frequently play a role in human diseases, but the process of…





















