Novel stem cell trial in heart failure patients to begin

The University of Pittsburgh Medical Center (UPMC) is beginning a clinical trial to evaluate the safety and feasibility of a potential treatment for congestive heart failure that involves injecting a patient’s own bone marrow-derived stem cells directly into the heart muscle. The procedure is expected to be performed in five to 10 patients who are scheduled to receive a heart assist device as a bridge to organ transplantation.
The stem cell trial is one of only a handful that has been cleared by the U.S. Food and Drug Administration (FDA) for heart disease. And because most patients in the UPMC study will eventually receive transplants, the trial represents the first time researchers will be able to examine a human heart treated with stem cells, an opportunity that should help solve some of the mystery as well as resolve scientific debate about just how it is that stem cells work to improve heart function.
Despite advances that have given rise to more effective medical and surgical therapies, including the use of heart assist devices, heart disease continues to exact an economic burden and be a major cause of death in the United States. As such, researchers have looked to the potential of stem cells as a treatment for congestive heart failure and other heart disease. Laboratory studies indicating that a subset of stem cells from bone marrow can generate new heart cells and blood vessels have spawned interest in performing clinical studies. While relatively few such studies have been conducted, and most have been done abroad, preliminary results have shown that blood flow and heart function improve in patients receiving the stem cell therapy.
However, to date, there has been no research in humans that helps explain why such improvements are seen, raising questions that have become the crux of scientific debate about the mechanism and action of these cells once introduced into the heart.
“People have questioned whether stem cells take on the functional characteristics of heart cells or blood vessels, or whether they help recruit other cells and growth factors that have the ability to help regenerate heart tissue. Our study presents the unique opportunity to examine the heart several months after stem cell injections, when the patient’s native heart is removed for organ transplantation, and we’re hopeful we’ll find the answers to everyone’s questions,” noted Amit N. Patel, M.D., M.S., principal investigator of the clinical trial and director of UPMC’s Center for Cardiac Cell Therapy. Dr. Patel also is director of the Center for Cardiovascular Cellular Therapy at the McGowan Institute for Regenerative Medicine.
UPMC plans to enroll five to 10 patients. To qualify, patients must have congestive heart failure and require implantation of a ventricular assist device (VAD) as a bridge to transplantation.
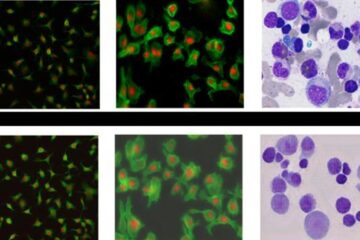
Unlike the other FDA-approved trials, surgeons will not deliver the cells through a catheter leading into the heart’s coronary arteries but will instead inject them directly into the diseased heart tissue during the VAD implant surgical procedure. With the patient under anesthesia, Dr. Patel’s team will harvest bone marrow from the patient’s hipbone, and the cells believed to have the greatest therapeutic benefit, CD34+ cells, will be isolated. About three hours later, once the VAD has been implanted and connected to the heart’s main pumping chamber, the ventricle, the cells, together with a small amount of the patient’s blood plasma, will be injected into about 25 to 30 sites of the diseased heart in a process taking no more than five minutes. Depending on their weight, each patient will receive between 25 and 45 million stem cells.
In order to help the researchers better understand what effects the stem cells have on the cellular structures that surround the injection sites, they also will give patients injections containing only plasma to a different area of the heart. That way, once the native heart is removed, pathologists will be able to compare the differences between tissue samples from both areas, as well as make comparisons to tissue samples removed during routine biopsies, which are done at the time of the VAD implantation.
Co-principal investigator of the trial is Robert L. Kormos, M.D., professor of surgery at the University of Pittsburgh School of Medicine, director of UPMC’s Artificial Heart Program and medical director of the McGowan Institute for Regenerative Medicine.
Media Contact
More Information:
http://www.upmc.eduAll latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles

Bringing bio-inspired robots to life
Nebraska researcher Eric Markvicka gets NSF CAREER Award to pursue manufacture of novel materials for soft robotics and stretchable electronics. Engineers are increasingly eager to develop robots that mimic the…

Bella moths use poison to attract mates
Scientists are closer to finding out how. Pyrrolizidine alkaloids are as bitter and toxic as they are hard to pronounce. They’re produced by several different types of plants and are…
AI tool creates ‘synthetic’ images of cells
…for enhanced microscopy analysis. Observing individual cells through microscopes can reveal a range of important cell biological phenomena that frequently play a role in human diseases, but the process of…





















