Interspecies Transplant Works in First Step for New Diabetes Therapy

In the first step toward animal-to-human transplants of insulin-producing cells for people with type 1 diabetes, Northwestern Medicine® scientists have successfully transplanted islets, the cells that produce insulin, from one species to another. And the islets survived without immunosuppressive drugs.
Northwestern scientists developed a new method that prevented rejection of the islets, a huge problem in transplants between species, called xenotransplantation.
“This is the first time that an interspecies transplant of islet cells has been achieved for an indefinite period of time without the use of immunosuppressive drugs,” said study co-senior author Stephen Miller. “It’s a big step forward.”
“Our ultimate goal is to be able to transplant pig islets into humans, but we have to take baby steps,” said Xunrong Luo, M.D., also co-senior author of the study that will be published online July 12 in the journal Diabetes. “Pig islets produce insulin that controls blood sugar in humans.”
Luo is an associate professor of nephrology at Northwestern University Feinberg School of Medicine and medical director of the Human Islet Cell Transplantation Program at Northwestern Memorial Hospital. Miller is the Judy Gugenheim Research Professor of Microbiology-Immunology at Feinberg.
For people with hard-to-control type 1 diabetes, a transplant of insulin-producing islets from a deceased donor is one important way to control their chronic disease, in which their bodies do not produce insulin. However, there is a severe shortage of islet cells from deceased donors. Many patients on waiting lists don’t receive the transplant or suffer damage to their heart, nerves, eyes and kidneys while they wait.
Using islets from another species would provide wider access to transplants for humans and solve the problem. But concerns about controlling rejection of transplants from a different species have made that approach seem insurmountable until now.
In the new study, scientists persuaded the immune systems of mice to recognize rat islets as their own and not reject them. Notably, the method did not require the long-term use of drugs to suppress the immune system, which have serious side effects. The islets lived and produced insulin in the mice for at least 300 days, which is as long as scientists followed the mice.
While the barrier from rats to mice is probably lower than from pigs to humans, the study showed interspecies islet transplants are possible and without immunosuppressive drugs, Luo said.
In the study, the rat splenocytes, a type of white blood cell located in the spleen, were removed and treated with a chemical that caused their deaths. Next, the dead splenocytes were injected into the mice. The cells entered the spleen and liver and were mopped up by scavenger cells. The scavengers processed the splenocytes and presented fragments of them on their cell surface, triggering a reaction that told the T cells to accept the subsequently transplanted rat islets and not attack them.
But rejection was still a threat. A unique challenge of an interspecies transplant is controlling the B cells, immune cells that are major producers of antibodies. Initially, when scientists transplanted the rat islets into the mice, the mouse immune system started producing antibodies against the rat cells causing rejection.
To solve the problem, Luo realized she needed to kill off the B-cells at the same time she injected the donor islets into the mice. Thus, she gave the mice B-cell depleting antibodies — already used in a clinical setting in human transplants. When the B-cells naturally returned after the transplant, they no longer attacked the rat islets.
“With this method, 100 percent of the islets survived indefinitely,” Luo said. “Now we’re trying to figure out why the B-cells are different when they come back.”
The study lead author is Shusen Wang, formerly a postdoctoral student in Luo’s lab.
The research was supported by the JDRF and National Institutes of Health Directors New Innovator Award DP2 DK083099.
Media Contact
More Information:
http://www.northwestern.eduAll latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles
Making diamonds at ambient pressure
Scientists develop novel liquid metal alloy system to synthesize diamond under moderate conditions. Did you know that 99% of synthetic diamonds are currently produced using high-pressure and high-temperature (HPHT) methods?[2]…
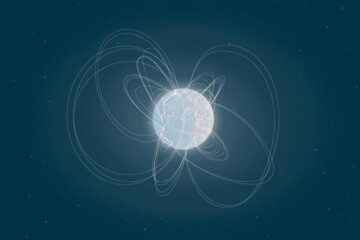
Eruption of mega-magnetic star lights up nearby galaxy
Thanks to ESA satellites, an international team including UNIGE researchers has detected a giant eruption coming from a magnetar, an extremely magnetic neutron star. While ESA’s satellite INTEGRAL was observing…
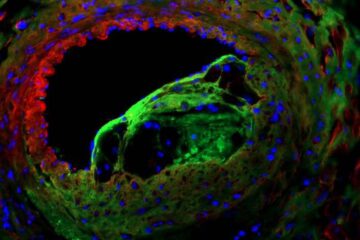
Solving the riddle of the sphingolipids in coronary artery disease
Weill Cornell Medicine investigators have uncovered a way to unleash in blood vessels the protective effects of a type of fat-related molecule known as a sphingolipid, suggesting a promising new…





















