Brain protein central to both Parkinson's, drug addiction identified

Scientists have identified a protein that appears not only to be central to the process that causes Parkinson's disease but could also play a role in muting the high from methamphetamine and other addictive drugs.
The action of the protein, known as organic cation transporter 3 or oct3, fills a longstanding gap in scientists' understanding of the brain damage that causes symptoms like tremor, stiffness, slowness of movement and postural instability. While these are found mainly in patients with Parkinson's disease, there are more than three dozen other known causes of this array of symptoms, known as “parkinsonism.”
In a paper published online this week in the Proceedings of the National Academy of Sciences, scientists at Columbia University Medical Center and the University of Rochester Medical Center have shown that oct3, a protein that shepherds molecules into and out of cells, plays a critical role, bringing toxic chemicals to the doorstep of the brain cells that die in patients with Parkinson's disease. The team found that oct3 is involved in the brain's response to addictive drugs like methamphetamine as well.
Precisely what causes Parkinson's disease remains largely a mystery. Some cases have a known genetic basis, and most others are attributed to environmental causes or a combination of gene-environment interactions. Doctors know that symptoms of Parkinson's stem from the death of a very small, specialized group of brain cells known as dopamine neurons, which produce a chemical needed by another area of the brain to help us move freely. It's not until most of those brain cells have already died that patients begin to show symptoms.
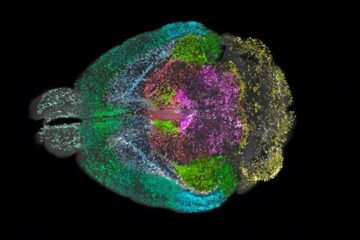
For decades, scientists have been trying to understand why those cells die. The latest paper supports a role for astrocytes, a type of cell that is the most common in the brain but which has been often overlooked by scientists focused more on cells known as neurons that send electrical signals. Astrocytes' role in Parkinson's is no surprise to brain experts who have also identified them as a player in Alzheimer's disease, amyotrophic lateral sclerosis, epilepsy, and other diseases.
“Astrocytes are definitely much more than support cells in the brain,” said Kim Tieu, Ph.D., a corresponding author of the paper and assistant professor in the Department of Environmental Medicine at the University of Rochester Medical Center. “Scientists are discovering their involvement in many diseases. The latest results point to their role in Parkinson's disease.”
Tieu initiated the study while a post-doctoral research associate in the laboratory of Serge Przedborski, M.D., Ph.D., the Page and William Black Professor of Neurology at Columbia University and a corresponding author. They chose to study how the brain handles a chemical known as MPTP, which ultimately damages the exact same brain cells that are injured in patients with Parkinson's disease. While MPTP does not cause Parkinson's disease, scientists regularly use it as a model for the disease because it causes an identical type of brain damage.
In the brain, MPTP is converted primarily in astrocytes to a chemical called MPP+, which is deadly to dopamine neurons. More than 20 years ago, as a graduate student with Solomon Snyder, M.D., Jonathan Javitch, M.D., Ph.D., now professor of psychiatry and pharmacology at Columbia and an author on the current paper, concluded that MPP+ is released from astrocytes before it kills dopaminergic neurons. But exactly how MPP+ is freed from astrocytes was unknown.
In this week's PNAS paper, the scientists finger oct3 as the shepherd that escorts toxic MPP+ out of the astrocytes and into the space surrounding dopamine neurons. That's where another molecule known as the dopamine transporter picks it up and brings it into the neuron itself.
When the team blocked or genetically removed oct3 in mice, the dopamine neurons in the brains did not die despite the presence of MPTP in the brain. Without oct3, MPP+ remained sequestered inside astrocytes and did not affect the dopamine neurons. And when oct3 was present in the usual amounts, dopamine neurons died as expected.
“The neurons affected in Parkinson's disease don't live in isolation in the brain,” said Przedborski. “You must understand the brain environment as a whole to understand disease. For many years, people had a neuron-centric view of neurodegenerative diseases. But more and more scientists are realizing that if you wish to understand the process of neurodegeneration, you must take into account the astrocytes, the microglia, as well as the neurons. Astrocytes maintain an intimate relationship with neurons, and to understand one, you have to understand the other.”
The team also analyzed brain tissue from people who died of Parkinson's disease and found that oct3 is active in astrocytes in the brain region affected by Parkinson's disease. They found the same thing in mice, where the absence of oct3 correlated exactly to areas of the brain where neurons were not damaged.
The team also showed that oct3 plays a role in the brain's response to methamphetamine. Oct3 is critical for helping astrocytes soak up excess dopamine in the space around neurons. When dopamine isn't removed as quickly or thoroughly as usual, people can feel euphoric, but they can also experience brain damage. The finding that oct3 may play a role matches other scientists' observations that people in whom oct3 activity is reduced have a higher potential for addiction.
The molecule might also offer a new target for treating depression. Many anti-depressants work by allowing the brain chemical serotonin to stay available in the brain longer than it otherwise would. Since one of oct3's functions is to remove serotonin from the brain, blocking it may offer a new avenue to treat depression.
The chemicals that the team used to block oct3 in mice would be toxic in people, and there is no drug available for people now that blocks or boosts oct3, Tieu and Przedborski said. But such a drug might be useful for Parkinson's, drug addiction, and depression.
“How you choose to manipulate the function of oct3 depends on the source of the toxic molecules,” said Tieu, who is also a scientist in the University's Center for Neural Development and Disease. “You would try to lessen its effects in a condition where it makes a toxic molecule available to vulnerable cells, as illustrated in the current model of Parkinson's disease. But in the case of drug addiction, you might try to increase it, to lessen the impact of a drug like methamphetamine.”
Other authors at the University of Rochester include post-doctoral research associates Mei Cui, Ph.D., Radha Aras, Ph.D., and Mamata Hatwar, Ph.D.; graduate student Whitney Christian; medical and graduate student Phillip Rappold; former undergraduate student Joseph Panza; and Ned Ballatori, Ph.D., professor of environmental medicine. At Columbia, Vernice Jackson-Lewis, Ph.D., associate research scientist, also contributed to the research. The work was funded by the National Institute of Environmental Health Sciences.
Columbia University Medical Center provides international leadership in basic, pre-clinical and clinical research, in medical and health sciences education, and in patient care. The medical center trains future leaders and includes the dedicated work of many physicians, scientists, public health professionals, dentists, and nurses at the College of Physicians and Surgeons, the Mailman School of Public Health, the College of Dental Medicine, the School of Nursing, the biomedical departments of the Graduate School of Arts and Sciences, and allied research centers and institutions. Established in 1767, Columbia's College of Physicians and Surgeons was the first institution in the country to grant the M.D. degree and is now among the most selective medical schools in the country. Columbia University Medical Center is home to the most comprehensive medical research enterprise in New York City and state and one of the largest in the United States. Columbia University Medical Center is affiliated with NewYork-Presbyterian Hospital, the nation's largest not-for-profit hospital provider.
Media Contact
All latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles
Advanced Brain Science Without Coding Expertise
Researchers at Helmholtz Munich and the LMU University Hospital Munich introduce DELiVR, offering a new AI-based approach to the complex task of brain cell mapping. The deep learning tool democratizes…

Bringing bio-inspired robots to life
Nebraska researcher Eric Markvicka gets NSF CAREER Award to pursue manufacture of novel materials for soft robotics and stretchable electronics. Engineers are increasingly eager to develop robots that mimic the…

Bella moths use poison to attract mates
Scientists are closer to finding out how. Pyrrolizidine alkaloids are as bitter and toxic as they are hard to pronounce. They’re produced by several different types of plants and are…





















