Antibodies reverse type 1 diabetes in new immunotherapy study
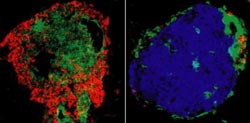
This image shows T cells (red, green) not detected and insulin (blue) readily observed in pancreatic islets of antibody-treated (Right) VS.untreated (Left) diabetic NOD mouse. Credit: Tisch Lab, UNC-Chapel Hill<br>
The findings, published online ahead of print (June 29, 2012) in the journal Diabetes, suggest for the first time that using a short course of immunotherapy may someday be of value for reversing the onset of Type I diabetes in recently diagnosed people. This form of diabetes, formerly known as insulin-dependent diabetes mellitus, is an autoimmune disease in which the body's own immune T cells target and destroy insulin-producing beta cells in the pancreas.
The immune system consists of T cells that are required for maintaining immunity against different bacterial and viral pathogens. In people who develop Type 1 diabetes, “autoreactive” T cells that actively destroy beta cells are not kept in check as they are in healthy people.
Senior study author Roland Tisch, PhD, professor of microbiology and immunology at UNC, said a need for effective immunotherapies also exists to treat Type 1 diabetes in people already living with the disease.
“Clinically, there have been some promising results using so-called depleting antibodies in recently diagnosed Type 1 diabetic patients, but the disease process is blocked for only a short period of time,” Tisch said. “These antibodies don't discriminate between T cells normally required for maintaining immunity to disease-causing pathogens and the autoreactive T cells. Therefore T cells involved in maintaining normal immune function are also going to be depleted.
“You're getting some efficacy from immunotherapy but its only transient, it doesn't reverse the disease, and there are various complications associated with the use of these depleting antibodies.”
Tisch said his UNC lab has been studying the use of certain “non-depleting antibodies.” These bind to particular proteins known as CD4 and CD8 expressed by all T cells. Just as the name implies, when these non-depleting antibodies selectively bind to CD4 and CD8 they don't destroy the T cells; the overall numbers of T cells are unaffected.
With this in mind Tisch wanted to determine whether these non-depleting antibodies could have a therapeutic effect in the non-obese diabetic, or NOD mouse, an excellent model for human Type 1 diabetes.
The answer is yes. In some of the recently diagnosed NOD mice, blood sugar levels returned to normal within 48 hours of treatment. Within five days, about 80 percent of the animals had undergone diabetes remission, reversal of clinical diabetes.
“The protective effect is very rapid, and once established, is long-term,” he said. “We followed the animals in excess of 400 days after the two antibody treatments, and the majority remained free of diabetes. And although the antibodies are cleared from within the animals in 2-3 weeks after treatment, the protective effect persists.” The study showed that beta cells in the NOD mice had been rescued from ongoing autoimmune destruction.
In looking for the mechanism to explain how the therapy worked, the researchers found that the antibodies had a very selective effect on T cells that mediated beta cell destruction. After treatment, “all the T cells that we would normally see in the pancreas or in tissues associated with the pancreas had been purged,” said Tisch. This despite the fact that the numbers of T cells found in other tissues and blood were unaffected.
The researchers also found an increase in the numbers of “immune regulatory” T cells. In the healthy individual, these regulatory T cells block autoimmunity, Tisch explained. “They protect us from the autoreactive cells that all of us have. And that's why most of us don't develop autoimmune diseases such as Type 1 diabetes.”
“We've demonstrated that the use of non-depleting antibodies is very robust. We're now generating and plan to test antibodies that are specific for the human version of the CD4 and CD8 molecules.”
UNC study coauthors with Tisch are first-author, Zuoan Li, (now at the University of Iowa); Ramiro Diz, Aaron Martin, Yves Maurice Morillon, Douglas E. Kline, (now at the University of Chicago); Li Li (now at Harvard Medical School); and Bo Wang.
Support for research came from the National Institute of Diabetes and Digestive and Kidney Diseases, part of the National Institutes of Health; and from the Juvenile Diabetes Research Foundation.
Media Contact
More Information:
http://www.unc.eduAll latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles

Combatting disruptive ‘noise’ in quantum communication
In a significant milestone for quantum communication technology, an experiment has demonstrated how networks can be leveraged to combat disruptive ‘noise’ in quantum communications. The international effort led by researchers…
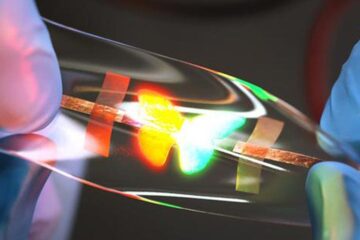
Stretchable quantum dot display
Intrinsically stretchable quantum dot-based light-emitting diodes achieved record-breaking performance. A team of South Korean scientists led by Professor KIM Dae-Hyeong of the Center for Nanoparticle Research within the Institute for…

Internet can achieve quantum speed with light saved as sound
Researchers at the University of Copenhagen’s Niels Bohr Institute have developed a new way to create quantum memory: A small drum can store data sent with light in its sonic…





















