Going Intrastromal: Refractive Surgery from the Inside Out
In the ongoing search for better ways to perform refractive surgery, the advent of femtosecond lasers capable of operating within the cornea has led to several new surgical approaches.
Two of the most interesting currently under investigation use femtosecond lasers to alter the cornea intrastromally, producing results comparable to—or better than—those produced by LASIK, with fewer potential risks and complications. One procedure cuts a lenticule within the stroma which is then removed; another alters the stromal tissue and adjusts the refraction without the need for any tissue removal or cutting of the cornea at all.
Here, two surgeons with extensive experience using these procedures discuss the advantages and disadvantages of each and share their thoughts about what the future may hold.
Staying Inside the Stroma
The second intrastromal procedure under investigation at several sites around the world, known as intraCOR, is completely different. In intraCOR, the Femtec femtosecond laser (20/10 Perfect Vision) is used to alter the biomechanical properties and shape of the cornea—not necessarily its thickness—by using photodisruption to cause changes inside the stroma. No tissue is removed; no flap or lenticule are created; the anterior and posterior surfaces of the cornea remain intact; and the procedure doesn’t disturb the epithelium or Bowman’s layer. As a result, many problems associated with opening the cornea or ablating epithelium are avoided.
Luis Ruiz, MD, of Bogotá, Colombia, has performed refractive surgery for 33 years and has extensive experience with the new procedure. “IntraCOR remodels the cornea by changing the biomechanical forces inside it,” he explains. “I’ve treated presbyopia for the past 14 years, and our initial effort using this new approach is to treat presbyopia by creating corneal multifocality. For a hyperope, we steepen the cornea in the 2- to 3-mm central zone, creating a myopic zone. This doesn’t affect distance vision at all but dramatically improves near vision. So far we’ve treated about 1,300 eyes, including presbyopic, myopic, astigmatic and hyperopic eyes. About 600 of those were treated just for presbyopia. “The most amazing thing about this surgery is that it’s extremely simple,” he continues. “Performing the surgery for presbyopia takes between 20 and 25 seconds and recovery is very fast. The stromal cells are converted into bubbles; within 1.5 to 2 hours, the bubbles disappear. At that point the patient starts seeing very well. And in many patients it’s almost impossible to tell that they have had any kind of surgery. We thought that maybe after one month vision would deteriorate a little, but we’ve followed 20 or 30 eyes for a year now, and their vision is exactly the same. If anything, near vision improves a little with time.” Dr. Ruiz reiterates that the procedure primarily changes the shape of the cornea rather than the thickness. “We don’t do anything to reduce corneal thickness,” he notes. “For example, suppose you have a central cornea with a steepness of about 43 D preop and a peripheral steepness of 42 D at the edge of the 4-mm optical zone. After surgery, the central zone is 44 or 45 D, but the peripheral region stays the same.
“All of these patients are really happy,” he adds. “They don’t need a long follow-up; they go back to work the next day without any problems. They don’t need a lot of medications. In fact, at this point we’re just giving these patients tears—we never use antibiotic or anti-inflammatory drops.” Dr. Ruiz says they do use cyclosporine, however, starting before the surgery. “We’re dealing with patients who are mostly over 50 years old,” he points out. “The quality of their tear film is not as good, and quality of vision seems to be a tiny bit sharper when we use cyclosporine. Also, in the early postop period, presbyopic patients have some haloes and myopic patients have some glare at night. However, with cyclosporine, they complain much less and the symptoms disappear much more quickly. This is a recent discovery, so we need a longer follow-up. But it looks like another way to improve outcomes.”
Refining the Procedure
Dr. Ruiz says that a big part of their current work is creating a nomogram so the procedure will be equally effective for both easy and difficult eyes. “We’re examining patients extensively with a WaveScan, iTrace, OPD-Scan, Ocular Response Analyzer, Pentacam and other devices, to gather as much information as possible,” he explains. “This will help us determine what information is most useful when deciding which patients are the best candidates. We’ve found, for example, that when the posterior surface of the cornea is very aspheric the cornea takes the correction readily. If it’s not as aspheric, it requires more surgery to have the same effect.”
One of the factors being measured is corneal hysteresis, to see whether having a different hysteresis preop changes the outcome, and how much the procedure itself affects hysteresis. “So far, we haven’t seen a big difference in outcome in a patient with a preop hysteresis of 11 compared to a patient with a hysteresis of 9.5,” notes Dr. Ruiz. “But we’ve discovered that the procedure itself has a minimal effect on corneal hysteresis, in contrast to LASIK. LASIK can reduce hysteresis from 9.5 to 6; this procedure hasn’t reduced hysteresis by more than 0.2 or 0.3. In many cases the change is even less. “Unfortunately, there’s no agreement yet out exactly what hysteresis is measuring, but right now it’s the only tool we have for gauging how strong the cornea is preop vs. postop. The difference compared to LASIK is striking.”
Who Is a Candidate?
Dr. Ruiz notes that the range of correction he is currently treating (beyond just treating for presbyopia) is very small. “Up to now, we’ve only corrected very low myopia—up to 0.5 or 0.75 D,” he says. “With 1 D of myopia the patient improves for distance, but doesn’t usually get 20/20. With hyperopia, 2 or 2.5 D preop is the limit so far. We can treat astigmatism up to 2 D, but the outcomes are not as accurate as for those patients with a half diopter less than that. Our goal, of course, is to correct greater amounts of refractive error, but we’re taking it slowly.”
For now, larger corrections can be achieved by combining procedures or using the intrastromal procedure more than once. “We can do one surgery to correct hyperopia and another to correct presbyopia,” he says. “And we’ve treated some hyperopes needing 3 D of correction by enhancing the original treatment one, two or three months later using the same protocol. The end result is just as good. You can also do LASIK for the larger part of the correction and use this procedure to fine-tune the result.”
However, Dr. Ruiz notes that he has learned to be careful with patients who have previously had LASIK. “This procedure works well on some of these patients, but not all,” he says. “The flap seems to increase the effect of the procedure. As long as we don’t interact with the flap, we don’t seem to have any problem. Interestingly, patients who have previously had RK do quite well unless the earlier surgery corrected more than 4 D of myopia. We’ve done 20 or 30 eyes like this, and the results have been excellent—almost as good as the results on virgin eyes. That may be because the RK incisions were vertical, unlike a LASIK flap.” Dr. Ruiz says they are avoiding patients with irregular corneas for now. “The effect of the surgery in these patients is much greater,” he notes. “The surgery becomes unpredictable. But eventually, if we combine this procedure with cross-linking or other treatments, it may be possible to work with those patients as well.”
Intrastromal vs.
LASIK Dr. Ruiz points out several advantages that this procedure has relative to LASIK. “For one thing, our contrast sensitivity results are amazing,” he says. “Patients test better postop than preop. We never, ever see that in LASIK. Presbyopic LASIK leaves the cornea with different curves centrally and peripherally. That creates aberrations. Our procedure barely affects the corneal surface; the topography afterwards shows a very even surface. “Second,” he continues, “we don’t cut any important nerves in the cornea because we don’t create a flap. So the eye doesn’t lose any sensitivity, and creating dry eye is not an issue.
“Third, this procedure is safer, for several reasons,” he notes. “We don’t open the cornea, and because the instrument has a curved interface it doesn’t increase IOP the way a flat interface can. Also, the procedure is faster than LASIK. Treatment time for presbyopia is about 20 seconds; for presbyopia and myopia or hyperopia, about 40 seconds.” “I’ve worked with refractive surgery for 33 years, and I’ve never seen a surgery like this, with fast recovery and predictability,” he adds. “So far we’ve never had a patient end up with worse vision postop than preop. I can tell these patients that if they’re not happy, I’ll refund their money.
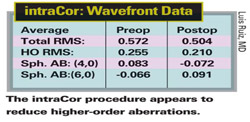
“Making a flap produces changes in the cornea that are very difficult to compensate for,” he notes. “This procedure, which doesn’t involve making a flap, has led to a reduction in higher-order aberrations, better refraction, better quality of vision and better contrast-sensitivity results than I’ve seen with any variation of LASIK—and I’ve performed all of them over the years. “For example, I have one patient who is a pilot in Central America,” he continues. “I performed presby-LASIK on one of his eyes two years ago; he was 20/20 and J1 afterwards. Recently, he returned and I used the new intrastromal procedure on his other eye, with several other surgeons in attendance. We examined him three hours after the surgery, and he said his vision in the intrastromal eye was definitely superior, even though his other eye is still 20/20 and J1. I believe the difference is the result of higher-order aberrations. A month later, he still prefers the second eye.
“Out of thousands of patients I’ve operated on, I’ve never seen a presby-LASIK patient who ended up with 20/15 distance vision and J2 or J1 near vision,” he adds. “With intraCOR, that result is common.”
What’s Next?
Dr. Ruiz looks forward to increasing the amount of refractive correction this procedure can generate. “I would say the current procedure can effectively treat presbyopia for those with refractive errors between -0.75 and +2 D,” he notes. “That’s probably 80 percent of the presbyopic population.
“In the future, we hope to be able to correct higher-order aberrations, especially in patients who have had previous refractive surgery,” he continues. “We know we can generate 1- or 2-ìm changes anywhere in the cornea. In the meantime, I look forward to many more surgeons using this procedure. Their data will help provide the proof that it really works.”
Starting in January 2009, 20/10 Perfect Vision was scheduled to begin working with Bausch & Lomb in a joint venture using this procedure. Meanwhile, Dr. Ruiz hopes that the procedure will receive the CE Mark in Europe by the middle of 2009. Dr. Sekundo’s research is supported by Carl Zeiss Meditec, but he is not a paid consultant. Dr. Ruiz has no current financial interest in intraCOR, although 20/10 Perfect Vision is covering the cost of exams and procedures while the procedure is developed.
Copyright© 2000 – 2009 Jobson Medical Information LLC unless otherwise noted. All rights reserved. Reproduction in whole or in part without permission is prohibited.
Media Contact
More Information:
http://www.technolaspv.comAll latest news from the category: Corporate News
Newest articles

Properties of new materials for microchips
… can now be measured well. Reseachers of Delft University of Technology demonstrated measuring performance properties of ultrathin silicon membranes. Making ever smaller and more powerful chips requires new ultrathin…

Floating solar’s potential
… to support sustainable development by addressing climate, water, and energy goals holistically. A new study published this week in Nature Energy raises the potential for floating solar photovoltaics (FPV)…

Skyrmions move at record speeds
… a step towards the computing of the future. An international research team led by scientists from the CNRS1 has discovered that the magnetic nanobubbles2 known as skyrmions can be…





















