Chili peppers and inflammation: Researchers unravel mechanism of pain sensitivity

Scientists at Massachusetts General Hospital (MGH) have discovered a common component to the burning sensation produced by chili peppers and the pain associated with arthritis. The finding, published in the September 26 issue of Neuron, could help scientists devise new strategies to block the pain hypersensitivity associated with inflammation.
“The receptor activated by chili peppers in the mouth and other tissues also increases in the terminals of sensory neurons in the skin after inflammation, and this contributes to pain hypersensitivity,” says Clifford Woolf, MD, PhD, director of the Neural Plasticity Research Group in the Department of Anesthesia and Critical Care at MGH. A receptor is a protein that transports a chemical signal into a cell.
Woolf and lead author Ru-Rong Ji, PhD, also of the MGH Neural Plasticity Research Group, found that the increased production of the receptor following inflammation is mediated by a signal molecule called p38, located within sensory neurons. The chili pepper receptor, which is technically called TRPV1, responds to capsaicin, the chemical that is responsible for the “hot” in peppers. It also responds to actual heat and to low pH, a condition that occurs with inflammation.
“With these findings, we’re starting to understand why patients with arthritis or other inflammatory conditions are likely to have increased pain and sensitivity to heat,” says Woolf. He and his research team were surprised to find that the activation of p38 can cause a twenty-fold increase in the amount of TRPV1 protein in the skin but not in the activity of the gene coding for TRPV1.
“This means that the chili pepper receptor is not being regulated by the gene being switched on but by more protein being produced, an unexpected form of regulation,” says Ji. He also notes that their findings will open up new options for pain management. “We could use an inhibitor to p38 to block the increase in TRPV1, therefore blocking pain in patients who suffer from many diseases and conditions that involve inflammation.”
Following inflammation, the activation of p38 is very precise. The scientists found that it is caused by a specific growth factor signal acting on a particular subset of pain sensory neurons. There are a variety of pain sensations that create different changes within neurons, and all of the signals that are generated have not yet been identified. Each new discovery, like the current finding by the MGH researchers, sheds light on these complex pathways and brings new treatment strategies closer.
Media Contact
More Information:
http://www.mgh.harvard.edu/All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Rocks with the oldest evidence yet of Earth’s magnetic field
The 3.7 billion-year-old rocks may extend the magnetic field’s age by 200 million years. Geologists at MIT and Oxford University have uncovered ancient rocks in Greenland that bear the oldest…
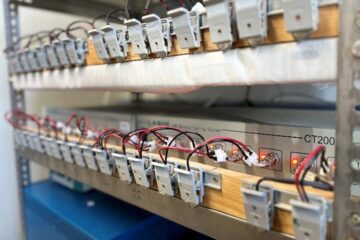
Decisive breakthrough for battery production
Storing and utilising energy with innovative sulphur-based cathodes. HU research team develops foundations for sustainable battery technology Electric vehicles and portable electronic devices such as laptops and mobile phones are…

Superradiant atoms could push the boundaries of how precisely time can be measured
Superradiant atoms can help us measure time more precisely than ever. In a new study, researchers from the University of Copenhagen present a new method for measuring the time interval,…





















