‘Killer’ cells used to combat rare cancer

Scientists from the University of Edinburgh are using immune cells harvested from blood donors to help fight an unusual cancer which can affect transplant patients. And their findings, published recently in The Lancet show that the therapy has proved effective in a number of cases. The treatment proved successful last year in saving the life of a four-year-old boy from Birmingham, who developed the cancer— post-transplant lympho-proliferative disease— following a liver and bowel transplant.
The technique, which involves boosting the patient’s own immune system to fight cancer without affecting the transplanted organ, can also be adapted to treat other virus infections, or AIDS patients who have developed lymphomas.
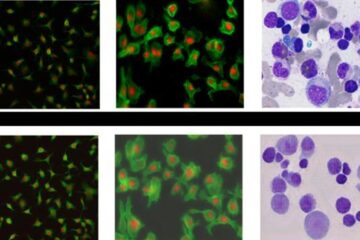
Clinical research scientist Dr Tanzina Haque explained: “The Epstein-Barr virus (EBV) is a common virus best known for causing glandular fever, and is carried by about 90% of the population, without a problem. When a patient receives an organ transplant, he or she is given immuno-suppressive drugs to stop the body rejecting the organ, but this also lowers their immunity to infections by removing the body’s ’killer’ cells, the cytotoxic T-lymphocytes. If a transplant patient’s immunity is compromised, EBV can infect cells called B-lymphocytes, causing them to grow in an uncontrolled way and become malignant. The resulting cancer can be fatal in up to 70% of cases.”
Dr Haque said that to reduce doses of immuno-suppressive drugs could cause organ transplant rejection, so the Edinburgh team, headed by Professor Dorothy Crawford and backed by funding from Cancer Research UK, devised a method of removing ‘killer’ cells from screened blood donations and tissue-type matching them to transplant patients. Should any patients develop lymphoma, they can be infused with matched cells from the bank containing more than 100 blood donations.
The technique, known as Cytotoxic T-Lymphocyte (CTL) Therapy, has shown to have no adverse side-effects for patients. Results published in The Lancet show of eight patients in the trial who were suitable for treatment, two died, five made a complete recovery, two did not respond and one showed a partial response. Two further patients died before their tumour response could be evaluated.
Dr Haque said this UK-wide multicentre clinical trial could not have been possible without the collaboration of the Scottish National Blood Transfusion Service, different transplant centers, and the many blood donors who helped by allowing their blood to be used for generating the T-cells.
Media Contact
More Information:
http://www.ed.ac.uk/news/All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Bringing bio-inspired robots to life
Nebraska researcher Eric Markvicka gets NSF CAREER Award to pursue manufacture of novel materials for soft robotics and stretchable electronics. Engineers are increasingly eager to develop robots that mimic the…

Bella moths use poison to attract mates
Scientists are closer to finding out how. Pyrrolizidine alkaloids are as bitter and toxic as they are hard to pronounce. They’re produced by several different types of plants and are…
AI tool creates ‘synthetic’ images of cells
…for enhanced microscopy analysis. Observing individual cells through microscopes can reveal a range of important cell biological phenomena that frequently play a role in human diseases, but the process of…





















