Stroke: When Helper Cells Become Harmful
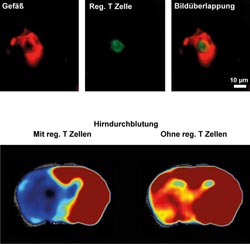
After a stroke, regulatory T cells (green) can be mainly identified in the cerebral vessels (red), where they interact with the vessel wall, clotting the respective blood vessel in the process (upper row of pictures). Accordingly, the cerebral blood flow (lower row of pictures) after a stroke is significantly higher in mice without regulatory T cells (right) than in normal mice (left). For measuring the cerebral blood flow, the animals were examined in an MRI scanner.<br>Picture: Christoph Kleinschnitz / Heinz Wiendl<br>
The course of a stroke was previously described by scientists as follows: A blood vessel supplying the brain with oxygen and vital nutrients is suddenly blocked by a blood clot. This leads to a stroke, causing injury to the brain. As a result, many patients suffer from neurological dysfunctions, such as severe paralysis or speech disorders.
“This picture must be supplemented by another important factor, namely the immune system,” says Professor Christoph Kleinschnitz, head of stroke medicine at the University of Würzburg's Department of Neurology. He verified this in a joint project with the study group of Professor Heinz Wiendl at the University Hospital of Münster.
Regulatory T cells as culprits
The new insight was discovered in mice the immune system of which lacks regulatory T cells due to a genetic defect: The brain damage sustained by these mice after a stroke is reduced by about 75 percent as compared to normal mice. Furthermore, these mice develop significantly fewer neurological dysfunctions.
Regulatory T helper cells are an important part of the immune system and usually have the task of suppressing excessive immune responses of the body. Due to their regulatory properties, they play a protective role in many diseases, such as multiple sclerosis or rheumatism.
Paradigm shift in immunology
“The fact that regulatory T cells aggravate the brain damage to this extent in acute stroke cases came as a complete surprise to us,” reports Heinz Wiendl, Director of the Department of Neurology, Division for Inflammatory Diseases of the Nervous System and Neuro-Oncology at the University Hospital of Münster: “We can say without exaggeration that this constitutes a paradigm shift from the perspective of immunology.”
In their research, the immunologists also investigated with which mechanisms the regulatory T cells exacerbate the harmful effect of a stroke. They found out that this cell type interacts with platelets and blood vessel walls, especially in the early stages after a stroke. This worsens the clotting of the cerebral vessels, further reducing the cerebral blood flow.
The next studies
The scientists are now going to determine whether the results can be applied to humans. Should this be the case, strokes might be treated in future with drugs that affect regulatory T cells.
“This would represent a small medical revolution,” says Kleinschnitz, for stroke is a widespread disease, having become the second leading cause of death worldwide. Effective therapies are scarce. “It will still take a series of further studies, however, to translate the discovery into an effective drug treatment,” Kleinschnitz emphasizes.
Sponsors of the research
The studies were funded by the German Research Foundation (DFG) and by the Else Kröner-Fresenius Foundation. The DFG supported the research via the excellence cluster “Cells in motion” in Münster and the collaborative research center 688 in Würzburg.
“Regulatory T cells are strong promoters of acute ischemic stroke in mice by inducing dysfunction of the cerebral microvasculature”, Christoph Kleinschnitz, Peter Kraft, Angela Dreykluft, Ina Hagedorn, Kerstin Göbel, Michael K Schuhmann, Friederike Langhauser, Xavier Helluy, Tobias Schwarz, Stefan Bittner, Christian T Mayer, Marc Brede, Csanad Varallyay, Mirko Pham, Martin Bendszus, Peter Jakob, Tim Magnus, Sven G Meuth, Yoichiro Iwakura, Alma Zernecke, Tim Sparwasser, Bernhard Nieswandt, Guido Stoll, Heinz Wiendl. Blood, published ahead of print November 15, 2012, doi:10.1182/blood-2012-04-426734
Contact persons
Prof. Dr. Christoph Kleinschnitz, Department of Neurology at the University Hospital of Würzburg, T (0931) 201-23756, christoph.kleinschnitz@uni-wuerzburg.de
or Prof. Dr. Heinz Wiendl, Department of Neurology – Division for Inflammatory Diseases of the Nervous System and Neuro-Oncology, University Hospital of Münster, T (0251) 83-46810, heinz.wiendl@ukmuenster.de
Media Contact
More Information:
http://www.ukmuenster.deAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Properties of new materials for microchips
… can now be measured well. Reseachers of Delft University of Technology demonstrated measuring performance properties of ultrathin silicon membranes. Making ever smaller and more powerful chips requires new ultrathin…

Floating solar’s potential
… to support sustainable development by addressing climate, water, and energy goals holistically. A new study published this week in Nature Energy raises the potential for floating solar photovoltaics (FPV)…

Skyrmions move at record speeds
… a step towards the computing of the future. An international research team led by scientists from the CNRS1 has discovered that the magnetic nanobubbles2 known as skyrmions can be…





















