First mouse lung transplants lay groundwork for new ways to prevent transplant rejection in humans

Ultimately, the mouse model could pave the way for developing new therapies to prevent lung transplant rejection – a major problem that limits the long-term success of the procedure. The mouse model is described in the June issue of the American Journal of Transplantation.
Five years after lung transplant surgery, only about 45 percent of patients are still alive, according to the U.S. Organ and Procurement and Transplantation Network. This compares with five-year survival rates of about 70 percent for heart and liver transplants and about 80 percent for kidney transplants. About 1,000 lung transplants are performed each year in the United States.
“The high failure rate of lung transplants is a huge problem,” says lung transplant surgeon Daniel Kreisel, M.D., Ph.D., an assistant professor of surgery and a lead investigator of the research. “Unlike other organs, lungs are constantly exposed to bacteria and viruses in the environment, and we think this exposure increases the risk of chronic rejection and the eventual failure of the organ. This is why the mouse model is so critical. It will allow us to understand the molecular mechanisms that control lung transplant rejection.”
Lung transplants are the only treatment option for end-stage lung disease, including chronic obstructive pulmonary disease (COPD), cystic fibrosis, pulmonary fibrosis and certain congenital lung defects. Following a transplant, patients must take drugs for the rest of their lives that suppress the immune system and prevent it from attacking the new lung. This leaves them vulnerable to upper respiratory infections, which can quickly develop into pneumonia.
Kreisel and others suspect that these illnesses alter the immune response and increase inflammation, which eventually lead to chronic rejection. They note that mainstay immunosuppressive drugs simply are not effective at preventing chronic rejection for lung transplants, and they hope the mouse model will reveal why.
“The current hypothesis is that lung transplant rejection is linked to chronic inflammation from transient viral or bacterial infections, and this can be aggravated by the fact that transplant recipients are taking immunosuppressive drugs,” Kreisel says.
Mouse models for heart, liver and kidney transplants have existed for years, but developing a similar model for lung transplantation has proved to be a real technical challenge. Mouse lungs measure less than an inch in length and the pulmonary vein and artery, which carry blood to and from the heart, are as thin as human hair.
Mikio Okazaki, M.D., a postdoctoral fellow, adapted the lung transplantation technique used in rats to the mice. He uses synthetic cuffs to join the donor vessels with those of the recipient. Okazaki has successfully performed several hundred lung transplants in the mice, and the team’s analysis indicates the model simulates the same immune response that occurs in humans following lung transplantation.
Before Okazaki and his Washington University colleagues developed the mouse model, researchers had been studying lung transplantation using a nonphysiological mouse model in which a small section of trachea from one mouse was transplanted under the skin of another. Although it was simple to create, the model did not accurately mimic lung transplantation. “It was a very artificial model that had little to do with reality, Okazaki says. “We think the new model will be far better for studying the underlying immune mechanisms that lead to rejection.”
The new mouse lung transplant model has an advantage over those in rats and larger animals because the genetics of mice are well documented and their genes are easier to manipulate. “With the mice, we can selectively delete genes to study their function in the transplanted lung or in the recipient, which we’ve not been able to do effectively in other animal models,” says Andrew Gelman, Ph.D., an assistant professor of surgery, who is a lead investigator of this research. “By understanding the genes that control lung graft survival, researchers will be able to better guide the development of therapies to counteract chronic rejection.”
The mouse model also will allow the researchers to investigate how other transplant-related complications affect the long-term success of the procedure. Many lung transplant patients experience gastric reflux, and doctors suspect this acid exposure damages the lining of the lung and further exposes the organ to pathogens. The mouse model will let researchers evaluate whether gastric reflux increases the risk of lung rejection.
Additionally, the time between surgery to harvest a donor lung and transplant it into a patient is widely suspected to affect its overall function after transplant surgery. The mouse model will help pinpoint the inflammation that underlies damage to the organ when it can’t be transplanted quickly and may lead to ways to prevent such injury.
Based on mouse models of other solid organ transplants, researchers have learned that different groups of immune cells contribute to rejection in different organs. “Rejection of the lung differs from rejection of the heart in terms of the cells that participate in that rejection,” says Alexander Sasha Krupnick, M.D., assistant professor of surgery. “Every organ is different. What we’ve learned about rejection of the heart in mice does not apply to lungs. So we are thrilled to finally have an acceptable mouse model of lung transplantation to help us discover ways to increase the success of these transplants in humans.”
Media Contact
More Information:
http://www.wustl.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
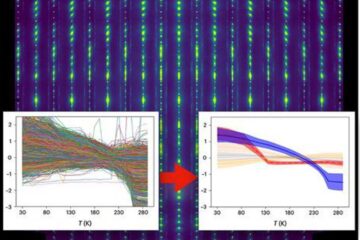
Machine learning algorithm reveals long-theorized glass phase in crystal
Scientists have found evidence of an elusive, glassy phase of matter that emerges when a crystal’s perfect internal pattern is disrupted. X-ray technology and machine learning converge to shed light…
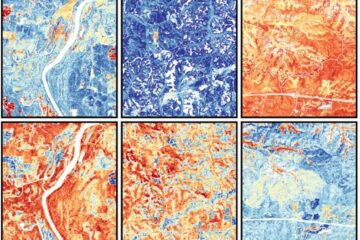
Mapping plant functional diversity from space
HKU ecologists revolutionize ecosystem monitoring with novel field-satellite integration. An international team of researchers, led by Professor Jin WU from the School of Biological Sciences at The University of Hong…

Inverters with constant full load capability
…enable an increase in the performance of electric drives. Overheating components significantly limit the performance of drivetrains in electric vehicles. Inverters in particular are subject to a high thermal load,…





















