Welsh medics to examine how surgery can cure diabetes

95% of morbidly obese people – those with a Body Mass Index of over 40 – have Type 2 diabetes, sometimes known as maturity-onset diabetes.
However, nearly 80% of patients who undergo gastric bypass surgery to reduce the size of their stomachs and small intestines find that their diabetes disappears within two to three days – before any weight loss has occurred.
Senior Clinical Lecturer Dr Jeffrey Stephens is leading the research at the School of Medicine’s Diabetes Research Group. He said: “Although patients with Type 2 diabetes do not always require insulin treatment, the average diabetic needs about 30 units of insulin a day to control blood sugar levels.
“For obese patients, this can rise to 200 units a day. To go from such a high level of insulin-dependency to not needing insulin in a matter of a few days is a dramatic result, and we need to understand the reasons why this happens.”
The research team, which includes Professor Steve Bain and Professor Rhys Williams from Swansea University’s School of Medicine, and Professor John Baxter, a bariatric surgeon with Swansea NHS Trust, are focusing attention on a protein known as Glucagon Like Peptide 1 (GLP-1), which is produced in the small intestine.
Dr Stephens said: “Overweight people who have Type 2 diabetes tend to have lower levels of GLP1 and we are investigating whether these levels return to normal after bariatric surgery. Basically, we want to know whether reducing the size of the small intestine and stomach restores production of GLP1, and why this should be the case.”
High blood sugar seen with poorly controlled diabetes may cause lethargy, excessive thirst and susceptibility to infection, and contributes to diabetic complications including premature heart disease, stroke, blindness, and gangrene.
“Bariatric surgery is not just effective in terms of controlling obesity. It clearly has other major health implications, with the potential to impact positively on Type 2 diabetes and other associated conditions. There is also the potential for the NHS to generate substantial savings in long term treatment costs,” added Dr Stephens.
“Not only will this research improve our understanding of why overweight people develop Type 2 diabetes, it may also lead to an effective, non-surgical treatment for those with the condition. We are immensely grateful to the BUPA Foundation for giving us this opportunity.”
Media Contact
More Information:
http://www.swansea.ac.uk/medicine/All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Bringing bio-inspired robots to life
Nebraska researcher Eric Markvicka gets NSF CAREER Award to pursue manufacture of novel materials for soft robotics and stretchable electronics. Engineers are increasingly eager to develop robots that mimic the…

Bella moths use poison to attract mates
Scientists are closer to finding out how. Pyrrolizidine alkaloids are as bitter and toxic as they are hard to pronounce. They’re produced by several different types of plants and are…
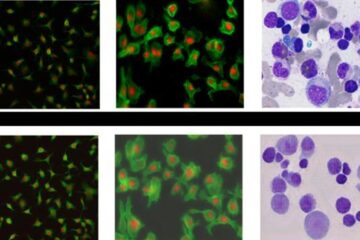
AI tool creates ‘synthetic’ images of cells
…for enhanced microscopy analysis. Observing individual cells through microscopes can reveal a range of important cell biological phenomena that frequently play a role in human diseases, but the process of…





















