First-ever genomic test predicts which lung cancer patients need chemotherapy to live

The test has the potential to save thousands of lives each year by recommending chemotherapy for patients who are currently advised against it, said the test's developers at Duke's Institute for Genome Sciences & Policy.
The test's promising results have initiated a landmark multi-center clinical trial, to be led by Duke investigators next year. Patients with early-stage non-small cell lung cancer, the most common and fatal form of cancer, will receive the genomic test and its results will determine their treatment.
The new test, called the Lung Metagene Predictor, scans thousands of genes to identify patterns of gene activity in individual tumors that indicate a patient is likely to suffer a recurrence of disease. Recurrent tumors are typically fatal, so identifying at-risk patients is critical to properly treating them, said the Duke researchers.
“Using the unique genomic signatures from each tumor, our new test predicted with up to 90 percent accuracy which early-stage lung cancer patients would suffer a recurrence of their cancer and which patients would not,” said Anil Potti, M.D., an assistant professor of medicine and lead author of the study. “We now have a tool that can be used to move these high-risk patients from the 'no chemotherapy' group into the aggressive treatment group.”
The researchers will publish their findings in the Aug. 10, 2006, issue of the New England Journal of Medicine. The research was funded by the National Institutes of Health.
The genomic test can theoretically apply to any cancer, but the Duke team focused its effort on lung cancer because the survival rate is just 15 percent. Lung cancer now kills more Americans each year than breast, prostate and colorectal cancers combined. But toxic chemotherapy drugs are prescribed only to patients with relatively large and aggressive tumors.
Early-stage patients – those with small, stationary tumors – are considered at low risk of recurrence. Hence, they only receive surgery but not chemotherapy. The dilemma, said Potti, is that a third or more of early-stage patients who appear to be at low risk will experience a recurrent tumor.
“Until now, there simply has been no way to identify the 30 percent to 40 percent of early-stage lung cancer patients who would experience a recurrence,” Potti said. “Now, with our test, we can say with confidence that we can identify this group of patients so they can be treated accordingly.”
The upcoming trial is the first to use a genomic test to select treatment options for individual lung cancer patients, said David Harpole, M.D., a professor of thoracic surgery at Duke and principal investigator of the upcoming clinical trial. The trial, to begin within six months, will enroll more than 1,000 patients at multiple centers in the United States and Canada.
“If we can use the test to increase patient survival by even 5 percent, we would save 10,000 lives a year,” Harpole said.
The Duke researchers developed the test by analyzing the activity of genes from early-stage lung cancer patients whose disease outcomes were known. The Duke scientists then validated the genomic test in 129 patients by comparing the test's predictions with the patient's actual outcomes. The test predicted their risk of recurrence with 90 percent accuracy, the study showed.
If proven to be effective in the clinical trial, the test will replace the current method of assessing risk, which is imprecise and provides only a broad estimate of a patient's risk, said Joseph Nevins, Ph.D., a professor of molecular genetics at Duke and senior author of the study being reported.
Physicians now assign each patient to a clinical “stage” based on the size of the patient's tumor, whether it has invaded lymph nodes and whether it has spread to other organs. They use this staging method to prescribe the best treatment options. But staging parameters are general, at best, and do not accurately define who should receive chemotherapy, Nevins said.
“Instead of placing all patients with small tumors in the same early-stage category, as physicians currently would do, we can now assess their risk based on the tumor's genomic profile,” Nevins said. “The current system of 'staging' lung cancer tumors will eventually become obsolete.”
To employ the test, physicians take a sample of the tumor as it is removed during surgery. They extract its “messenger RNA,” which represents the activity of thousands of genes in the tumor. Messenger RNA translates a gene's DNA code into proteins that run the cell's activities. Hence, it is a barometer of a gene's activity level inside the cell.
Scientists label the messenger RNA with fluorescent tags. The fluorescent RNA is then placed on a tiny glass slide, called a gene chip. There, it binds to its complementary DNA sequence on the gene chip.
When scanned with special light, the fluorescent RNA emits a telltale luminescence that demonstrates how much RNA is present on the chip – and thus which genes are most active in a given tumor. The physicians then use a rigorous statistical analysis to assess the relative risk of large grouping of genes, called metagenes, which have similar characteristics.
The test generates a risk “number” for each patient. If their risk exceeds 50 percent, the patient is advised to get chemotherapy.
“This new genomic test is a clear example of personalized medicine, where we use the unique molecular characteristics of each patient's tumor to guide treatment decisions,” said Geoffrey Ginsburg, M.D., Ph.D., a professor of medicine and co-author of the study.
Eventually, physicians will use genomic tests not only to predict patient outcomes, but also to select the individual drugs that will best match a tumor's molecular makeup, Ginsburg said.
Media Contact
More Information:
http://www.duke.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
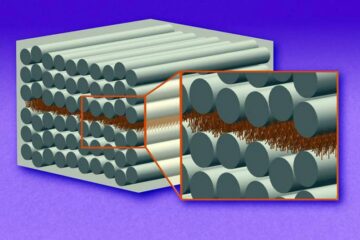
“Nanostitches” enable lighter and tougher composite materials
In research that may lead to next-generation airplanes and spacecraft, MIT engineers used carbon nanotubes to prevent cracking in multilayered composites. To save on fuel and reduce aircraft emissions, engineers…

Trash to treasure
Researchers turn metal waste into catalyst for hydrogen. Scientists have found a way to transform metal waste into a highly efficient catalyst to make hydrogen from water, a discovery that…
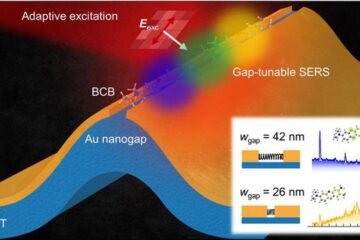
Real-time detection of infectious disease viruses
… by searching for molecular fingerprinting. A research team consisting of Professor Kyoung-Duck Park and Taeyoung Moon and Huitae Joo, PhD candidates, from the Department of Physics at Pohang University…





















