Optimal adjuvant radiation therapy associated with improved survival, meta-analysis shows

A new analysis of adjuvant radiation therapy in women with breast cancer following mastectomy is associated with better survival as measured at 10 years when appropriate doses and fields of radiation are used. The study was published in the January 4 issue of the Journal of the National Cancer Institute . The finding helps resolve controversy over whether radiation therapy improves both survival and risk of recurrence in women with operable breast cancer.
Past studies of radiation therapy in women with operable breast cancer have led to the conclusion that radiation therapy reduces the risk of recurrence of breast cancer but the effects on overall survival have been less clear. However, in some clinical trials, radiation therapy was given in inadequate or excessive doses or did not target an appropriate amount of tissue, including the chest wall and lymph nodes.
Val Gebski, of the National Health and Medical Research Council Clinical Trials Centre in New South Wales, Australia, and colleagues reanalyzed results from 36 clinical trials in which the use of radiation therapy was the sole difference between treatments given to breast cancer patients. They divided trials into three categories: category 1, for studies that used optimal radiation doses delivered to an appropriate amount of tissue; category 2, for studies where patients received an inadequate or excessive dose of radiation; and category 3, for studies in which an inadequate amount of tissue was treated with radiation therapy.
At 5 years, patients in category 1 studies had a 2.9% absolute increase in survival with radiation therapy than without. At 10 years, patients in category 1 studies had a 6.4% absolute increase in survival. In category 2 and 3 studies, radiation therapy was not associated with a difference in overall survival after 5 or 10 years of follow-up. Gebski and colleagues conclude that optimal radiation therapy improves patient survival, measured at both 5 and 10 years, and recommend that postmasectomy radiation therapy be considered for all patients at high risk.
Leonard R. Prosnitz, M.D., and Lawrence B. Marks, M.D., of Duke University Medical Center in Durham, N.C., in an accompanying editorial, praise the authors’ report, “It seems like such a simple idea. It is surprising that no one has ever done it before.” Prosnitz and Marks suggest that, despite the limitations of the meta-analysis format used, the results show that the quality of radiation therapy positively affects survival outcomes. They write, “The evidence is now strong for survival benefits for both postmastectomy radiation therapy and postlumpectomy radiation therapy.”
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Superradiant atoms could push the boundaries of how precisely time can be measured
Superradiant atoms can help us measure time more precisely than ever. In a new study, researchers from the University of Copenhagen present a new method for measuring the time interval,…
Ion thermoelectric conversion devices for near room temperature
The electrode sheet of the thermoelectric device consists of ionic hydrogel, which is sandwiched between the electrodes to form, and the Prussian blue on the electrode undergoes a redox reaction…
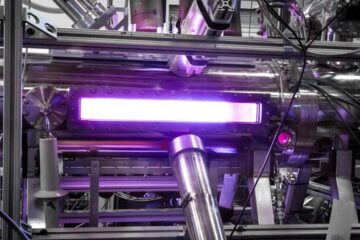
Zap Energy achieves 37-million-degree temperatures in a compact device
New publication reports record electron temperatures for a small-scale, sheared-flow-stabilized Z-pinch fusion device. In the nine decades since humans first produced fusion reactions, only a few fusion technologies have demonstrated…





















