New imaging method shows early in treatment if brain cancer therapy is effective

Diffusion MRI is good early predictor of whether cancer will progress
A special type of MRI scan that measures the movement of water molecules through the brain can help doctors determine halfway through treatment whether it will successfully shrink the tumor or a patient’s cancer will continue to grow, a new study shows. The test identifies after only three weeks of treatment – more than two months earlier than traditional tests — who is responding to the chemotherapy or radiation.
Researchers at the University of Michigan Comprehensive Cancer Center developed the assessment, which they call a functional diffusion map. They used a magnetic resonance imaging scan that tracks the diffusion, or movement, of water through the brain and mapped the changes in diffusion from the start of therapy to three weeks later. The tumor cells restrict the movement of water, so as those cells die, water diffusion changes.
In the study of 34 people with a type of brain tumor called high grade glioma, the researchers found that they could predict after three weeks, based on the functional diffusion map, which cancers would respond to the treatment and which cancers would continue to grow. These predictions corresponded to a significant difference in how long the patients lived.
Results of the study appear the week of Oct. 31 in the early online edition of the Proceedings of the National Academy of Sciences.
High grade gliomas have a high mortality rate, with people surviving only an average of 12 months after diagnosis. Typically, patients receive six to seven weeks of treatment, followed by a traditional MRI scan six weeks after completing therapy to determine if the tumor shrank. If the cancer did not respond to the treatment, a new approach may be tried.
“An early measure of tumor response such as this functional diffusion map could help doctors identify during the course of treatment who might benefit from a second-line therapy, sparing patients from a grueling treatment regimen that’s not working,” says senior study author Brian Ross, Ph.D., professor of radiology and biological chemistry at the U-M Medical School and co-director of the Molecular Imaging Program at the U-M Comprehensive Cancer Center. “Just as importantly, this finding opens up the opportunity to study not only if treatment is unsuccessful, but where in the tumor it is not succeeding. If this is the case, we can use our sophisticated radiation planning techniques to target higher radiation doses to the regions that are not responding,” says study author Theodore Lawrence, M.D., Ph.D., Isadore Lampe Professor and Chair of Radiation Oncology at the U-M Medical School.
In the study, 34 participants with late-stage diffuse high grade glioma, a type of brain tumor, underwent diffusion MRI before beginning a new treatment involving chemotherapy, radiation therapy or a combination. Three weeks later, they had another diffusion MRI. Eight to ten weeks after that, the participants underwent standard MRI to determine whether their tumor responded to the therapy.
At three weeks into treatment – more than two months before the final MRI scan – researchers could identify which patients would have a response to therapy over those with progressive disease. This corresponded to patients’ survival, with those classified as having progressive disease living an average 8.2 months while those with a response to treatment lived an average 18.2 months.
In addition, the time until the cancer began to progress was later in the group classified at three weeks by the functional diffusion map as having a partial response or stable disease, 7.3 months compared to 4.3 months for those identified as having progressive disease.
The researchers also looked at standard predictive factors of whether a patient is likely to do well on a therapy – factors such as age, tumor location and tumor size – but found the functional diffusion map was the only accurate predictor of overall survival.
“When the median survival for this type of cancer is less than 52 weeks, waiting an extra 10 weeks to know if treatment is working is a significant amount of time. We hope that functional diffusion mapping will eventually allow oncologists to manage each patient’s treatment based on real time evaluation of cellular response to therapy,” says study author Suresh Mukherji, M.D., professor of radiology and otolaryngology and division director of neuroradiology at the U-M Medical School.
The researchers believe the test may be useful for other types of cancer, including breast, head and neck, rectal, prostate and liver. The functional diffusion map is not yet available for routine use in clinic.
Additional U-M study authors are Daniel Hamstra, M.D., a resident in radiation oncology; Thomas Chenevert, Ph.D., professor of radiology; Bradford Moffat, Ph.D., assistant professor of radiology; Timothy Johnson, Ph.D., adjunct assistant professor and assistant research scientist in biostatistics; Charles Meyer, Ph.D., professor of radiology; Douglas Quint, M.D., professor of radiology; Stephen Gebarski, M.D., professor of radiology; Xiaoying Fan, a research technician in radiology; Christina Tsien, M.D., assistant professor in radiation oncology; Larry Junck, M.D., professor of neurology; and Alnawaz Rehemtulla, Ph.D., associate professor of radiation oncology and radiology.
Funding for the study was from the National Cancer Institute and the Charles A. Dana Foundation.
The University of Michigan holds a patent on this MRI diffusion technology and has licensed the commercialization rights to Molecular Therapeutics of Ann Arbor, in which Ross and Rehemtulla have a financial interest. A diffusion MRI can be performed on a standard MRI machine using a special workstation to compute the diffusion map. A workstation is being developed by Cedara Software Corp. of Ontario, Canada. Ross, Rehemtulla and Chenevert, as inventors of this technology, would stand to benefit financially from any commercial products.
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
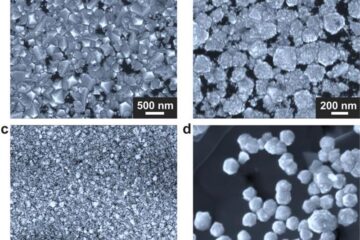
Making diamonds at ambient pressure
Scientists develop novel liquid metal alloy system to synthesize diamond under moderate conditions. Did you know that 99% of synthetic diamonds are currently produced using high-pressure and high-temperature (HPHT) methods?[2]…
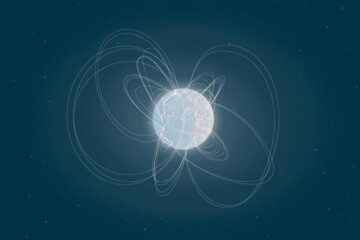
Eruption of mega-magnetic star lights up nearby galaxy
Thanks to ESA satellites, an international team including UNIGE researchers has detected a giant eruption coming from a magnetar, an extremely magnetic neutron star. While ESA’s satellite INTEGRAL was observing…
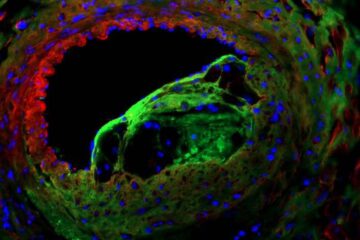
Solving the riddle of the sphingolipids in coronary artery disease
Weill Cornell Medicine investigators have uncovered a way to unleash in blood vessels the protective effects of a type of fat-related molecule known as a sphingolipid, suggesting a promising new…





















