Why some lung cancers stop responding to Tarceva and Iressa

Researchers at Memorial Sloan-Kettering Cancer Center (MSKCC) have found an explanation for why some lung cancers stop responding to the drugs erlotinib (TarcevaTM) and gefitinib (Iressa®). This discovery may lead to the development of new therapies to use when these agents stop working. The research is to be published online in the open-access international journal PLoS Medicine on February 22, 2005.*
Gefitinib and erlotinib are so-called targeted therapies, in that they halt the growth of certain cancers by zeroing in on a signaling molecule critical to the survival of those cancer cells. The two drugs are effective in about 10 percent of US patients with non-small cell lung cancer (NSCLC). Previous work from this group at MSKCC and from groups at Harvard Medical School showed that the two drugs work specifically in patients whose cancers contain mutations in a gene that encodes the epidermal growth factor receptor (EGFR). The MSKCC team has also shown that lung cancer patients with these mutations are often people who have never smoked.
“Although these targeted therapies are initially effective in this subset of patients, the drugs eventually stop working, and the tumors begin to grow again. We call this acquired or secondary resistance,” said Vincent A. Miller, MD, a thoracic oncologist at MSKCC and one of the study’s two lead authors. “This is different from primary resistance, which means that the drugs never work at all,” Dr. Miller said.
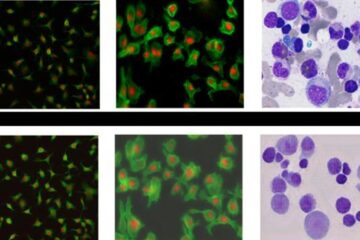
The study involved six patients who had received treatment with gefitinib or erlotinib and who later developed acquired resistance. Researchers studied samples taken from the patients’ tumors at different times before and during treatment. All of the tumors had the kinds of mutations in the EGFR gene that were previously associated with responsiveness to these drugs. But, in three of the six patients, they found that tumors that grew despite continued therapy had an additional mutation in the EGFR gene, strongly implying that the second mutation was the cause of drug resistance. Further biochemical studies showed that this second EGFR mutation, which was the same in all three tumors, could confer resistance to the EGFR mutants normally sensitive to these drugs.
“It is especially interesting that the mutation we found is strictly analogous to a mutation that makes other kinds of tumors resistant to another targeted therapy, imatinib mesylate (Gleevec®),” said Harold Varmus, President of MSKCC and senior author of the study. “Acquired resistance to Gleevec is a well-known problem, and understanding its molecular causes has led to the design of other drugs that overcome that resistance,” Dr. Varmus said. Imatinib mesylate is used to treat chronic myelogenous leukemia (CML), a stomach tumor called gastrointestinal stromal tumor (GIST), and other tumors caused by mutations in signaling enzymes like EGFR.
Non-small cell lung cancer makes up about 80 percent of all lung cancers. Mutations in a gene called KRAS (pronounced KAY-rass),which encodes a signaling protein activated by EGFR, are found in 15 to 30 percent of these cancers. The presence of a mutated KRAS gene in a biopsy sample is associated with primary resistance to these drugs, as reported by the same group of MSKCC investigators in the January, 2005, issue of PLoS Medicine. At this time there is no targeted therapy for patients with KRAS mutations.
“Tumor cells from patients in our study who developed secondary resistance to gefitinib and erlotinib after an initial response on therapy did not have mutations in KRAS. Rather, these tumor cells had new mutations in EGFR. This further indicates that secondary resistance is very different from primary resistance,” said William Pao, MD, PhD, a molecular biologist and thoracic oncologist and the study’s other lead author. “We are now trying to figure out other possible reasons why gefitinib or erlotinib stop working. We also hope to identify mutations in other potential cancer-causing genes that are critical for lung cancers to survive. Even though many mutated oncogenes have already been found, the crucial genes are still unaccounted for in about 50 percent of non-small cell cancers,” Dr. Pao said.
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Bringing bio-inspired robots to life
Nebraska researcher Eric Markvicka gets NSF CAREER Award to pursue manufacture of novel materials for soft robotics and stretchable electronics. Engineers are increasingly eager to develop robots that mimic the…

Bella moths use poison to attract mates
Scientists are closer to finding out how. Pyrrolizidine alkaloids are as bitter and toxic as they are hard to pronounce. They’re produced by several different types of plants and are…
AI tool creates ‘synthetic’ images of cells
…for enhanced microscopy analysis. Observing individual cells through microscopes can reveal a range of important cell biological phenomena that frequently play a role in human diseases, but the process of…





















