PET/MRI scans may help unravel mechanisms of prenatal drug damage

Scientists have demonstrated a new way to assess the potentially damaging effects of prenatal drug exposure–a technique that could also be used to monitor a fetus’s response to therapeutic drugs–using sophisticated, noninvasive medical imaging tools. Scientists at the U.S. Department of Energy’s Brookhaven National Laboratory, whose findings are reported in the February issue of the Society of Nuclear Medicine’s Journal of Nuclear Medicine, used positron emission tomography (PET) combined with magnetic resonance imaging (MRI) to track the uptake and distribution of trace amounts of cocaine in pregnant monkeys and found significant differences in where and how fast the drug accumulates in maternal and fetal organs.
“Understanding how drugs are transferred between a mother and her fetus during pregnancy may help us unravel the mechanisms of the drug’s damaging effects on unborn children,” said SNM member Helene Benveniste, M.D., Ph.D., chair of Brookhaven’s medical department in Upton, N.Y., and lead author of the paper, “Maternal and Fetal 11C-Cocaine Uptake and Kinetics Measured In Vivo by Combined PET and MRI in Pregnant Nonhuman Primates.”
“While studies that follow human drug abusers and their children over decades provide valuable information, animal studies can more quickly provide clues to the underlying mechanisms of damage and suggest ways to test new treatment or prevention strategies,” said Benveniste.
The imaging tools could also be used to assess the effects of therapeutic drugs, such as administering synthetic narcotics to pregnant women following surgical procedures performed on fetuses in utero. “Following such surgeries, which are becoming more common to correct congenital malformations, the mother is treated with narcotics for pain–and anesthesiologists are relying on the mother transferring the pain medication to the fetus via the placenta. But we actually do not know if what we give is sufficient to ’satisfy’ the pain level of the fetus,” said Benveniste, who is also a professor of anesthesiology at Stony Brook University.
Though other scientists have attempted to use PET to noninvasively monitor maternal-fetal drug exchange and pharmacokinetics (how quickly a drug is taken up and distributed among the body’s organs), the PET technique alone did not provide adequate anatomical detail of the tiny fetal organs. The current study combined PET with high-resolution magnetic resonance imaging (MRI) to track cocaine pharmacokinetics down to the level of the placenta and individual regions of the fetal brain.
“The MRI images, which have the necessary detail, served as a high-resolution anatomical template onto which we ’overlaid’ the PET pharmacokinetic data using sophisticated computer techniques,” Benveniste said. “The resulting images gave us the best of both worlds and allowed us to look at cocaine uptake and distribution in the mother and fetus simultaneously,” she added.
The animals were anesthetized prior to scanning. MRI scans were performed first, followed by PET. For the PET study, each animal was injected with a trace quantity of cocaine–less than 10 micrograms, which is not enough to cause pharmacological effects. The injected cocaine had previously been “labeled,” or “tagged,” with a short-lived radioactive form of carbon (carbon-11). This radiotracer emits a signal that is picked up by the PET scanner, which takes snapshots of the tracer’s location over time to show how much and how quickly the cocaine (and/or the metabolic byproducts that retain the carbon-11) enters and clears the various organs. The radiotracer decays and completely clears from the animal’s body in about two hours. After the procedure, the animals were returned to their social colony to deliver their offspring.
The combined images show that cocaine and/or its labeled metabolites readily cross the placenta. But the cocaine uptake distribution pattern observed in the fetus was very different from that of the mother. For example, mothers showed rapid uptake and clearance of the drug in the heart, kidneys and lungs, with slower uptake in the liver and brain. In the fetus, cocaine accumulated at the highest levels in the liver (due to the unique anatomy of fetal circulation) and to a lesser extent in the brain.
“While the uptake of the tracer into the fetal brain is lower and slower than in the mother’s brain, a measurable quantity of cocaine and/or its labeled metabolites does accumulate in the fetal brain, particularly in the striatum, where cocaine is known to bind to cell-surface receptors that result in a euphoric response,” Benveniste said.
The high uptake of radiolabeled cocaine in the placenta is also particularly relevant, the researchers said, because cocaine is known to constrict blood vessels in the placenta. It may be that this constriction of placental blood flow is one of the mechanisms underlying the harmful effects of cocaine exposure during pregnancy.
The research was funded by the Office of Biological and Environmental Research within the Department of Energy’s Office of Science and the National Institute on Drug Abuse. The monkeys were obtained from the Primate Laboratory, department of psychiatry, at the State University of New York (SUNY) Downstate, Brooklyn.
“Maternal and Fetal 11C-Cocaine Uptake and Kinetics Measured In Vivo by Combined PET and MRI in Pregnant Nonhuman Primates” was written by Benveniste; Joanna S. Fowler, Ph.D., William Rooney, Ph.D., and SNM member Yu-Shin Ding, Ph.D., all with Brookhaven’s chemistry department; Angela L. Baumann, M.D., Brookhaven’s medical department and the anesthesiology department of Stony Brook University; Daryn H. Moller, M.D., anesthesiology department, Stony Brook University; Congwu Du, Ph.D., Brookhaven’s medical department; Walter Backus, M.D., anesthesiology department, Stony Brook University; Jean Logan, Ph.D., and Pauline Carter, RN, both with Brookhaven’s chemistry department; Jeremy D. Coplan, M.D., psychiatry department, SUNY Downstate, Brooklyn; Anat Biegon, Ph.D., Brookhaven’s medical department; Leonard Rosenblum, Ph.D., and Bruce Scharf, DVM, both with the psychiatry department, SUNY Downstate, Brooklyn; John S. Gatley, Ph.D., Brookhaven’s medical department; and SNM member Nora D. Volkow, M.D., National Institute on Alcohol Abuse and Alcoholism, National Institutes of Health, Bethesda, Md.
Media Contact
More Information:
http://www.snm.orgAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
Silicon Carbide Innovation Alliance to drive industrial-scale semiconductor work
Known for its ability to withstand extreme environments and high voltages, silicon carbide (SiC) is a semiconducting material made up of silicon and carbon atoms arranged into crystals that is…
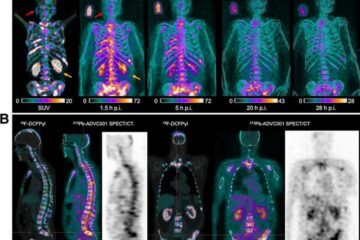
New SPECT/CT technique shows impressive biomarker identification
…offers increased access for prostate cancer patients. A novel SPECT/CT acquisition method can accurately detect radiopharmaceutical biodistribution in a convenient manner for prostate cancer patients, opening the door for more…

How 3D printers can give robots a soft touch
Soft skin coverings and touch sensors have emerged as a promising feature for robots that are both safer and more intuitive for human interaction, but they are expensive and difficult…





















