Tracing the life cycle of a manmade disease

MGH surgeon tells 40-year tale of investigation and innovation into the challenge of hip implant failure
A remarkable story of how a new disease was inadvertently caused by successful medical treatment, ultimately understood, and eventually defeated by scientific innovation is being told a major player in the process. In the December issue of Clinical Orthopedics and Related Research, William Harris, MD, DSc, of Massachusetts General Hospital (MGH), describes how the development of total hip replacement led to an unexpected problem, erosion of bone adjacent to the implant, and how his team and others both identified the process underlying that breakdown and helped to develop new materials that avoid the problem. “The history of the unraveling and prevention of this worldwide, unique, severe disease is a fascinating story of the integration of surgical innovation, molecular biology and material science,” writes Harris, who is Alan Gerry Clinical Professor of Orthopaedic Surgery at Harvard Medical School.
Harris was a pioneer in the field of joint replacement, beginning in the late 1960s. But he and other surgeons gradually observed that hip implants could loosen starting about 5 years after surgery and eventually fail completely. There were many theories about the cause of that loosening, several which focused on the adhesive used or the possibility of infection.
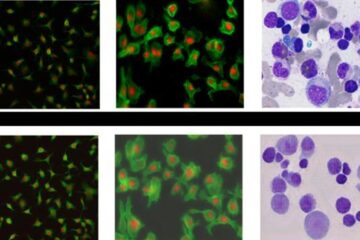
In 1976 Harris reported that implant failures appeared to be caused by a biological response at the site of the implant, which resulted in erosion of the bone. Looking further into the complication, Harris and colleagues found that, when the metal head of the implant rubbed against the polyethylene joint socket, small particles of polyethylene broke off over time. As the immune system reacted against these foreign particles, eventually it would attack and destroy the bone tissue, loosening the implant to the point of failure. It turned out that this complication was an entirely new manmade disease called periprosthetic osteolysis – a condition spawned inadvertently by the medical pioneers who, in finding a treatment for debilitating hip disease, had created a whole new problem.
In the early 1990s, Harris and his team began to focus their attention on finding a way to decrease the wear and tear of the polyethylene cushion in the joint, with an ultimate goal of eliminating osteolysis. The team’s initial work involved designing a hip simulator that could accurately replicate the motions and forces of the human hip and measure the wear performance of the implant. The MGH group then turned to a team of polymer chemists from Massachusetts Institute of Technology (MIT) for help in figuring out just how to make a polyethylene cushion that would resist wear and erosion through years of constant motion and weight. They eventually found the solution by “crosslinking” the polyethylene, which involves using a high dose of irradiation to bond molecules more tightly together, producing a much stronger and more durable material. Out of this MGH-MIT collaboration emerged a highly crosslinked, ultra-high-molecular-weight polyethylene.
The research team improved and refined the material by putting it through a melting process to eliminate any free radicals that could cause oxidation and lead to the degradation of the implant material. The material continued to prove strong and reliable in several studies, showing virtually no wear even after being subjected to excessive use and intense abuse. In 1999, the FDA approved highly crosslinked polyethylene for use in implants, the manufacture of which has been licensed to Zimmer, Inc. In subsequent years, the compound has continued to hold up exceptionally well, improving the long-term outlook for patients and expanding the field of total joint replacement.
“The availability of implants with crosslinked polyetheylene has made a great deal of difference for patient care,” Harris says. “For example, we used to be reluctant to do total hip replacements in young people because of the long-term risk of periprosthetic osteolysis, which led to doing some less satisfactory types of procedures that only postponed the need for an total hip. While we are still careful about doing hip replacements in any patients, current evidence suggests that the incidence of osteolysis is extraordinarily low with the new implants, making the procedure appropriate for a broader range of patients.”
Peter L. Slavin, MD, MGH president, recently said of this accomplishment, “The key beneficiaries of this work are patients throughout the world who, thanks to Dr. Harris and his team, now have the chance to experience a better quality of life for a much longer time.”
Media Contact
More Information:
http://www.mgh.harvard.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Bringing bio-inspired robots to life
Nebraska researcher Eric Markvicka gets NSF CAREER Award to pursue manufacture of novel materials for soft robotics and stretchable electronics. Engineers are increasingly eager to develop robots that mimic the…

Bella moths use poison to attract mates
Scientists are closer to finding out how. Pyrrolizidine alkaloids are as bitter and toxic as they are hard to pronounce. They’re produced by several different types of plants and are…
AI tool creates ‘synthetic’ images of cells
…for enhanced microscopy analysis. Observing individual cells through microscopes can reveal a range of important cell biological phenomena that frequently play a role in human diseases, but the process of…





















