Researcher declares ’PSA era is over’ in predicting prostate cancer risk

The PSA test, commonly used as a screening tool for detecting prostate cancer, is now all but useless for predicting prostate cancer risk, according to Stanford University School of Medicine researchers. A study of prostate tissues collected over 20 years – from the time it first became standard to remove prostates in response to high PSA levels to the present – reveals that as a screen, the test now indicates nothing more than the size of the prostate gland.
“The PSA era is over in the United States,” said Thomas Stamey, MD, professor of urology and lead author of the study published in the October issue of the Journal of Urology. “Our study raises a very serious question of whether a man should even use the PSA test for prostate cancer screening any more.”
The PSA test measures prostate specific antigen, a protein normally produced by the prostate gland. Stamey published the original findings in 1987 in the New England Journal of Medicine showing that increased blood PSA levels could be used to indicate prostate cancer. However, through the years, Stamey has come to believe that the PSA test is actually not a useful predictor of the amount or severity of prostate cancer. He said elevated levels of that protein actually reflect a condition called benign prostatic hyperplasia, a harmless increase in prostate size.
Stamey explained the change in correlation over the years by noting that the tumors encountered 20 years ago were generally so large they generated PSA levels high enough to provide a reasonably good measure of cancer severity. Now that screening is more commonplace in this country, many cancers are being caught earlier and are usually smaller – not generating enough PSA to be a good indicator of severity.
Prostate cancer is the most common cancer in men. Stamey cited a 1996 study in which researchers examined the prostates of healthy men who died from trauma, finding that 8 percent of those in their 20s already had prostate cancer. The American Cancer Society estimates that nearly a quarter of a million cases of prostate cancer will be diagnosed in the United States this year alone, and one in six men will be diagnosed with the disease at some point in their lives. Stamey said prostate cancer is a disease “all men get if we live long enough. All you need is an excuse to biopsy the prostate and you are going to find cancer.”
However, the risk of dying from prostate cancer is very low compared with lung cancer, which is the leading cause of cancer-related death in men, he said. “Almost every man diagnosed with lung cancer dies of lung cancer, but only 226 out of every 100,000 men over the age of 65 dies of prostate cancer, which is a rate of .003 percent,” he said, referring to National Cancer Institute statistics.
Stamey explained the basic dilemma as such: men whose PSA levels are above 2 ng/ml frequently undergo biopsy, which will almost always find cancer, but this does not necessarily mean that prostate removal or radiation treatment is required. “What we didn’t know in the early years is that benign growth of the prostate is the most common cause of a PSA level between 1 and 10 ng/ml,” he said.
To figure out the PSA test’s usefulness in determining which cancers warrant radiation or surgery, Stamey and his team from Stanford’s Department of Urology set out to document what was actually found following prostate removal, such as the volume and the grade of the cancer – two indications of the cancer’s severity. They then compared those findings to aspects that could be determined prior to surgery, such as how many of the cancers could be felt by rectal examination and the patient’s blood PSA level.
For the study, they used prostate tissue samples collected by professor John McNeal, MD, who has examined more than 1,300 prostates removed by different urologists at Stanford in the last 20 years. The researchers divided McNeal’s data into four five-year periods between 1983 and 2004 and looked at the characteristics of each cancer. They found that over time, there was a substantial decrease in the correlation between PSA levels and the amount of prostate cancer – from 43 percent predictive ability in the first five-year group down to 2 percent in the most recent one.
However, the Stanford researchers concluded that the PSA test is quite accurate at indicating the size of the prostate gland, meaning that it is a direct measure of benign prostatic hyperplasia. And Stamey pointed out that it is still very useful for monitoring patients following prostate removal as an indicator of residual prostate cancer that has spread to other parts of the body. “Our job now is to stop removing every man’s prostate who has prostate cancer,” said Stamey. “We originally thought we were doing the right thing, but we are now figuring out how we went wrong. Some men need prostate treatment but certainly not all of them.”
If the PSA test is no longer useful, the question remains as to the best course for detecting prostate cancer. Stamey recommends a yearly digital rectal exam for all men over 50. “If a cancer is felt in the prostate during a rectal examination, it is always a significant cancer and certainly needs treatment,” he said.
Unfortunately, he added, even large cancers often cannot be felt during rectal examination. His group is currently working on finding a blood marker that could indicate more aggressive forms of the cancer that can invade the body.
Other researchers who contributed to this work are Mitchell Caldwell, Rosalie Nolley, Marci Hemenez and Joshua Downs. The study was funded by donations to Stamey’s Prostate Cancer Research Fund at Stanford.
Media Contact
More Information:
http://www.stanford.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
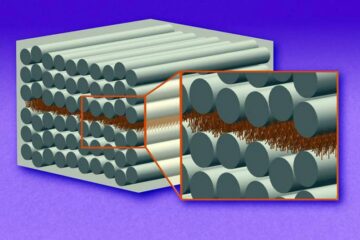
“Nanostitches” enable lighter and tougher composite materials
In research that may lead to next-generation airplanes and spacecraft, MIT engineers used carbon nanotubes to prevent cracking in multilayered composites. To save on fuel and reduce aircraft emissions, engineers…

Trash to treasure
Researchers turn metal waste into catalyst for hydrogen. Scientists have found a way to transform metal waste into a highly efficient catalyst to make hydrogen from water, a discovery that…
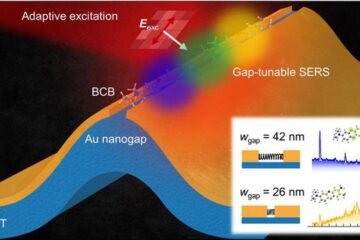
Real-time detection of infectious disease viruses
… by searching for molecular fingerprinting. A research team consisting of Professor Kyoung-Duck Park and Taeyoung Moon and Huitae Joo, PhD candidates, from the Department of Physics at Pohang University…





















