Dementia often undiagnosed in clinical settings

OHSU findings suggest more attention be paid to older patients’ cognitive functioning
Many older patients showing signs of dementia are not being diagnosed for the progressive brain disorder by their primary care physicians, an Oregon Health & Science University study has found.
The study, published in the current issue of the Journal of Gerontology: Medical Sciences, confirms previous research that found dementia often goes undiagnosed in primary care. It points to the need for heightened awareness among primary care physicians of the cognitive functioning of older patients, especially those experiencing adverse events that may be warning signs of dementia.
While the study was conducted in the Portland-metropolitan area, its results mirror that of previous studies showing the problem is internationally pervasive.
“It is surprising how widespread the lack of dementia diagnosis is, both throughout the United States and the world,” said lead author Linda Boise, Ph.D., M.P.H., assistant professor of neurology, OHSU School of Medicine, and director of education and information for the OHSU Layton Center for Aging & Alzheimer’s Disease Research. Protocols for recognizing dementia symptoms exist, but “doctors just need to use them.”
To study co-author Jeffrey Kaye, M.D., OHSU professor of neurology and the Layton Center’s director, the results show “our hard-working primary care physicians need help. They need time to adequately address cognitive problems. And they need a reimbursement system that recognizes the value of their time taken in detecting and managing cognitive impairment in our aging population.”
Researchers examined 553 patients of 34 primary care physicians affiliated with three Portland-area managed health care plans. Study subjects aged 75 and older were identified through primary care physicians to be contacted, and the study team assessed their cognitive functioning in their homes. Subjects were divided into three cognitive status groups: normal, mildly impaired and moderately-to-severely impaired; more than 43 percent were identified as cognitively impaired, including 29.7 percent classified as mildly impaired and 13.7 percent as moderately-to-severely impaired.
Researchers studied the medical charts of cognitively impaired individuals for evidence they were examined, diagnosed or treated for dementia, such as notes about symptoms, exams, discussions with family members, community resource referrals or dementia medication prescriptions.
Charts were analyzed for comments about adverse events in the last three years, such as medication use errors, problems complying with recommended treatments, increased emergency room visits, falls, family contacts with the doctor about a patient’s condition, missed appointments or frequent phone calls by the patient to the doctor.
These can, of course, be caused by conditions or factors other than dementia, so unless the doctor carries out a full inquiry into the reasons for these adverse events, he or she may not think to evaluate for possible dementia,” Boise said.
A contributing factor may be skepticism among physicians about the benefits of available treatments and the perception that nothing can be done for the patient, Boise said. “Of course, if the doctor works with the patient and family in a more comprehensive manner, there is a lot he can do to help the patient receive optimal care and promote optimal well-being.”
The study found that only 18 percent of mildly impaired patients and 34.8 percent of moderately-to-severely impaired patients were clinically evaluated for dementia, and that none of the mildly impaired patients and just 4.3 percent of the more severely impaired patients were offered dementia medication.
Moreover, nearly two-thirds – 61.6 percent – of the mildly impaired patients and three-fourths – 75.4 percent – of the more impaired individuals experienced one or more adverse events. Of those, only 23.7 percent of the mildly impaired group and 44.2 percent of the moderately-to-severely impaired group was evaluated for dementia.
Symptoms that can trigger a dementia assessment include difficulty with language, reasoning or spatial ability, and poor memory, including repetitiveness. Behavioral signs include difficulty with personal or family history, dressing inappropriately, and failing to appear for scheduled appointments or follow instructions.
Physicians may begin a dementia workup or exam when the patient’s family brings concerns about symptoms or behavioral signs to their attention. Falls and emergency room visits also trigger closer attention by the doctor. In fact, persons with dementia are at double the risk for falling as those without dementia due to changes in equilibrium and limb coordination, as well as inappropriate use of psychotropic, cardiac and analgesic drugs. They also are twice as likely as people their age to visit the emergency room.
According to the study, lagging dementia assessment in primary care could be due to the subtlety of dementia symptoms combined with the constraints of the clinical practice, such as the limited time available for evaluating patients.
“It is easy to miss mild dementia,” Boise said. “Older patients have a number of problems to attend to and they often don’t self-report memory problems. And social graces are preserved for a relatively long time over the course of dementia, so the patient might interact appropriately with the doctor. Thus, the doctor might not see anything to be concerned about.”
Other explanations are that physicians considered, but then discounted, that the adverse events should trigger a dementia assessment, or that they didn’t find a full clinical evaluation for dementia useful because they believe they could manage the dementia without assessing or identifying the cause.
“Doctors don’t see the imperative to conduct a complete evaluation for dementia,” Boise said. “The doctor may simply take into account that the older patient has some memory impairment and feel that they can manage care without full assessment.”
She said more research is needed to understand the potential harm to patients caused by the low rates of assessment, diagnosis and treatment for dementia.
“One area that I am concerned about is older patients who have chronic diseases that require careful self-management, such as diabetes,” Boise said. “We know that non-adherence to medication regimens is relatively common. How often is this due to dementia? We don’t really know.”
Early assessment could at least help families prepare emotionally for the tension and confusion that comes in a relationship with a loved one with dementia, Boise believes.
“Mostly what we hear from families is that they wish they had known sooner,” she said. “The person might be behaving in strange ways, often in ways that put them in the face of harm, such as non-payment of bills and getting lost, and the family doesn’t understand why.”
Kaye agreed. “Early diagnosis is important to help the family better understand and cope with changes that are frightening to them, and to develop proactive treatment plans,” he said. “There is also a very concrete potential benefit in reducing medical complications and costs. As the study showed, the failure to recognize cognitive impairment appears to be associated with increased medical complications such as medication errors, missed appointments and unnecessary emergency room visits.”
A dementia diagnosis also can be a weight off the shoulders of the patients, said study co-author Margaret Neal, Ph.D., professor of community health and director of the Institute on Aging at Portland State University.
“People who are experiencing the symptoms of dementia, as well as their families, are likely to be very worried about what is happening to them, and may well find it comforting to have an explanation,” Neal said.
Alzheimer’s disease is the most common form of dementia, according to the National Institute on Aging. As many as 4.5 million Americans suffer from the disease, which usually begins after age 60, with risk increasing with age. About 5 percent of men and women ages 65 to 74 and between 10 percent and 16 percent of those older than 75 have Alzheimer’s disease. Half of the 85-and-older population have the disease.
Media Contact
More Information:
http://www.ohsu.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
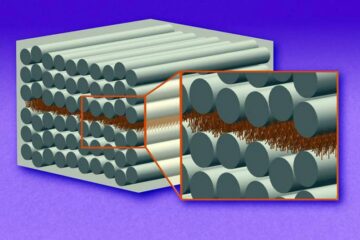
“Nanostitches” enable lighter and tougher composite materials
In research that may lead to next-generation airplanes and spacecraft, MIT engineers used carbon nanotubes to prevent cracking in multilayered composites. To save on fuel and reduce aircraft emissions, engineers…

Trash to treasure
Researchers turn metal waste into catalyst for hydrogen. Scientists have found a way to transform metal waste into a highly efficient catalyst to make hydrogen from water, a discovery that…
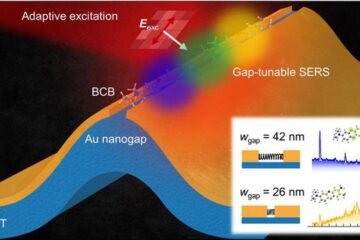
Real-time detection of infectious disease viruses
… by searching for molecular fingerprinting. A research team consisting of Professor Kyoung-Duck Park and Taeyoung Moon and Huitae Joo, PhD candidates, from the Department of Physics at Pohang University…





















