Patients’ cells from tumors, the immune system merged for customized cancer therapy

One of the strongest natural allies that cancer patients can tap to help fight tumor growth and metastasis may well be their own immune systems, and scientists affiliated with the Harvard University Medical School have devised ways of bolstering patients’ immune response against kidney and breast cancer.
In a paper published in the July 15 issue of the journal Clinical Cancer Research, the Harvard research team documented tumor regression in two breast cancer patients, and stabilization and containment of tumor growth in late stage breast and kidney patients through application of customized vaccinations made from the patients’ own tumor and immune system cells.
By fusing patients’ tumor cells with their immune system dendritic cells, researchers associated with the laboratory of Donald Kufe, M.D., professor of medicine at Dana-Farber Cancer Institute and Harvard Medical School, created customized antigen-presenting immune cells that train T cells to hunt, recognize and destroy the patients’ tumor cells.
“We aimed to develop a novel vaccine that took whole tumor cells with their complete array of tumor-specific antigens and combine them with the potent immune stimulating machinery of the dendritic cells,” said David Avigan, M.D., director of bone marrow transplantation at Beth Israel Deaconess Medical Center, and the lead author of the Clinical Cancer Research article.
The immune system develops T cells, which are white blood cells, to recognize foreign proteins, cells, and other matter that causes disease or infection. Tumor cells produce proteins, carbohydrates and other molecules that are different than the healthy cells that are normally found in the human body. The immune system can recognize cancer-related molecules, but cancer cells often are difficult for the immune system to detect. Conversely, dendritic cells are potent immune stimulating cells capable of generating the type of T Cells that attack and kill cancer cells.
In the past, immunologists have attempted to define cancer specific markers and develop vaccinations with those molecules, but most tumors don’t have well-defined antigens that can be isolated or have proved useful for vaccination development. Previous research approaches often were aimed at producing T cells that would recognize a defined cancer marker molecule, but the immune response to those vaccinations often fell short of expectations.
The Harvard team aimed at making a hybrid cell composed of both the cancer cells and dendritic cells taken from patients for use exclusively in the individual from whom the cells were obtained.
“This approach increased the number of antigens that immune system cells can recognize,” Avigan said. “And for the individual patients, those antigens are specific to their own tumor cells.”
The challenges of the trial included constructing the hybrid cells and evaluating the vaccinations performance in the donor patients. The dendritic cells were obtained from the patients’ blood. But harvesting cells from the tumors proved difficult. Cell numbers from individual patients were sometimes too low for successful generation of the hybrid tumor/dendritic cell fusion.
The study group included 23 patients–10 people with breast cancer and 13 with kidney cancer–from whom the researchers were able to collect enough cells to construct fusion cells in the laboratory. The effect of the vaccine on the patient’s immune system was measured by the number of circulating T cells that reacted with the patient-derived tumor cells before and after vaccination. Vaccination induced a doubling of tumor reactive T cells in about half the 18 patients in which this was measured. Ten patients doubled the percentage of CD4+ T cells that produced interferon gamma, a cytokine integral to the immune response. Seven patients doubled the percentage of CD8+ T cells that produced the interferon in response to exposure to the tumor.
“The increase of these interferon-producing T cells indicated that the fusion cell vaccination was promoting a heightened response by the immune system,” Avigan said. “That response was targeted at antigens on the tumor cells.”
The vaccine was well tolerated with only minimal toxicity observed. While a potential concern with vaccine therapy is the induction of an immune response against normal tissues of the body, no evidence of significant autoimmunity was seen.
A third of the study participants responded positively to the customized therapy. Among the breast cancer patient to be immunized, one woman responded to the trial vaccination with 80 percent regression of her chest wall tumor mass within a month. After four months, the tumor had regressed by 90 percent. She remained stable with no evidence of progression during the following two years. A second patient responded with regression of half a tumor that had spread to her adrenal gland, and almost half a pulmonary nodule as well. That individual showed resumed disease progression after a half year. A third breast cancer patient, and five kidney cancer patients, remained stable for three to nine months after completion of the vaccination treatments.
“The results from this patient group, while preliminary, hold promise that fusion cell technology may emerge as an effective immunotherapeutic strategy allowing patients to use their own immune system to fight their cancer,” Avigan said.
While the results were not universal to all the study participants, Avigan said that that further development of the vaccination, and application on patients with less advanced disease and whose immune systems were less severely weakened, may increase the positive results observed in the Harvard group’s initial Phase I trail.
Kufe’s and Avigan’s colleagues in the study were comprised of researchers from two Harvard Medical School teaching affiliates, the Dana-Farber Cancer Institute and Beth Israel Deaconess Medical Center.
Media Contact
More Information:
http://www.aacr.orgAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
Silicon Carbide Innovation Alliance to drive industrial-scale semiconductor work
Known for its ability to withstand extreme environments and high voltages, silicon carbide (SiC) is a semiconducting material made up of silicon and carbon atoms arranged into crystals that is…
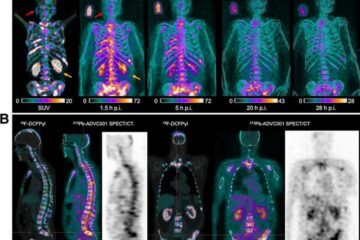
New SPECT/CT technique shows impressive biomarker identification
…offers increased access for prostate cancer patients. A novel SPECT/CT acquisition method can accurately detect radiopharmaceutical biodistribution in a convenient manner for prostate cancer patients, opening the door for more…

How 3D printers can give robots a soft touch
Soft skin coverings and touch sensors have emerged as a promising feature for robots that are both safer and more intuitive for human interaction, but they are expensive and difficult…





















