A new technique detects earliest signs of Alzheimer’s in healthy people

Brain researchers would dearly love to reliably identify changes in brain structure and metabolism associated with early Alzheimer’s disease — before symptoms emerge.
Such information would buy precious time and perhaps permit potential therapies to delay or even prevent the memory-robbing disease. Now, a new study by NYU School of Medicine researchers brings this goal one step closer to being realized.
Using a new technique to measure the volume of the brain, they were able to identify healthy individuals who would later develop memory impairment, a symptom associated with a high risk for future Alzheimer’s disease. The study is published in the December issue of the journal Radiology.
In the small study, led by Henry Rusinek, Ph.D., Associate Professor of Radiology at NYU School of Medicine, the researchers used MRI scans and a computational formula to measure a region of the brain called the medial-temporal lobe over a period of two years. This area contains the hippocampus and the entorhinal cortex, key structures allied with learning and memory. The researchers found that each year, this region of the brain shrank considerably more in people who developed memory problems compared with people who didn’t. The medial-temporal lobe holds about 30 cubic centimeters — the equivalent of one-sixth of a cup — of brain matter in each hemisphere of the brain.
“With our findings, we now know that the normal healthy brain undergoes a predictable shrinkage that can be used to help recognize Alzheimer’s several years before clinical symptoms emerge,” says Dr. Rusinek. “We believe this is the first MRI study to report these findings in healthy people, but it is only the first demonstration that extremely early diagnosis is possible, and the technique still requires additional work before it is ready for the clinic,” he adds.
The technique was about 90 percent accurate, meaning that it correctly predicted cognitive decline in nine out of 10 people, and it also correctly identified 90 percent of those whose memories would remain normally for their age.
However, the study only involved 45 people; future studies need to ascertain whether the technique would be as accurate in a much larger pool of subjects. In addition, it remains to be shown whether other neurodegenerative diseases that affect the aging brain can also be accurately identified with this technique.
“I believe that this technique opens an era of early diagnosis of Alzheimer’s disease,” says Mony J. de Leon, Ed.D., Professor of Psychiatry at NYU School of Medicine and one of the co-authors on the new study. “Now, we want to combine this technique with measurements of certain Alzheimer-related proteins found in the cerebrospinal fluid, to get an even more diagnostically specific assessment,” says Dr. de Leon, who is also Director of the Center for Brain Health at the William and Sylvia Silberstein Institute for Aging and Dementia at NYU and a research scientist at the Nathan Kline Institute, an affiliate of NYU School of Medicine, in Orangeburg, N.Y.
Alzheimer’s disease is a progressive illness that kills neurons in the brain, initially causing memory loss and eventually leading to dementia. It afflicts some four million older adults in the United States. Perhaps three times as many individuals suffer early-stage forms of the disease that incapacitate memory to one degree of another. Currently, the disease can be diagnosed definitively only after a person dies, by an autopsy showing certain brain abnormalities.
Previous research by NYU investigators and others has shown that MRI and PET imaging can reveal structural and metabolic changes in the brain that appear to point to early losses in memory and cognitive skills. For example, Dr. de Leon and his colleagues were the first to demonstrate with MRI scans that the hippocampus shrinks in people with mild cognitive impairment (MCI), a form of memory loss that often precedes Alzheimer’s.
Despite the promise of the MRI studies, the hippocampus is notoriously difficult to measure. Shaped like a sea horse and only about four centimeters long (shorter than a pinky), the brain structure yields its exact dimensions unwillingly. The entorhinal cortex is even smaller than the hippocampus, and it, too, is hard to discern clearly.
Faced with these challenges, Dr. Rusinek set out to devise a technique that would be more reliable than currently available methods for measuring atrophy in the region occupied by the hippocampus and entorhinal cortex. He based his technique on a mathematical algorithm created by British researchers for measuring the volume changes of the whole brain, and adapted it to measure a specific region of the brain: the medial-temporal lobe.
Dr. Rusinek reasoned that as long as he was measuring the brain area that contained the hippocampus and the entorhinal cortex, the other structures within his box were inconsequential. “His technique is like fishing with a net,” says Dr. de Leon. “The position of the fish in the net doesn’t matter. All that matters is that you are using a big enough net to catch a particular fish.”
The new study followed a group of 45 healthy men and women over the age of 60 for six years. At the beginning of the study, everyone was within the normal range on a battery of tests typically used to detect early loss of memory and other mental deficits. Each person received a baseline MRI scan, which was repeated two years later.
Thirteen of the people declined mentally over the course of the study, and six declined after the second MRI scan. Among those who declined, the rate of atrophy in the medial-temporal lobe was the most important variable that distinguished them from the normally aging individuals. The region lost about 0.7 percent of its volume annually — an amount smaller than the size of a pea. While in the normal aging subjects the region shrank by less than half that volume.
Dr. Rusinek is now attempting to improve the accuracy of the technique by measuring the volume of white and gray matter in the medial-temporal lobe and by improving the spatial resolutions of the MR images. White matter is the fatty insulation around the long, cable-like axons of neurons; gray matter contains the bodies of neurons. In a person with Alzheimer’s disease, the gray matter is largely destroyed. In future studies, Dr. Rusinek expects to find a greater loss of gray matter in people who are likely to develop the kind of cognitive impairment that precedes Alzheimer’s disease.
Media Contact
More Information:
http://www.med.nyu.edu/All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Optimising inventory management
Crateflow enables accurate AI-based demand forecasts. A key challenge for companies is to control overstock and understock while developing a supply chain that is resilient to disruptions. To address this,…

Cause of rare congenital lung malformations
Gene mutations in the RAS-MAPK signaling pathway disrupt lung development in the womb. Most rare diseases are congenital – including CPAM (congenital pulmonary airway malformations). These are airway malformations of…
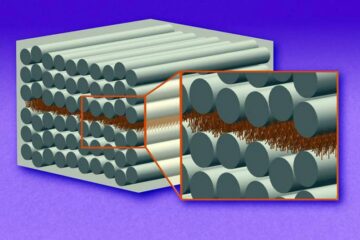
“Nanostitches” enable lighter and tougher composite materials
In research that may lead to next-generation airplanes and spacecraft, MIT engineers used carbon nanotubes to prevent cracking in multilayered composites. To save on fuel and reduce aircraft emissions, engineers…





















