Cedars-Sinai researchers detail events that enable brain tumors to weaken immune system

In an article appearing in a special issue of the Journal of Neuro-oncology, researchers at Cedars-Sinai Medical Center’s Maxine Dunitz Neurosurgical Institute describe a complex cell-level process that allows malignant brain tumors to protect themselves by damaging the thymus, rapidly degrading the immune system. In a second article, Institute scientists identify a molecular mechanism that causes cell death of cancer-fighting lymphocytes as they infiltrate a brain tumor.
“We are dissecting and better understanding the mechanisms that enable tumors to evade destruction by the immune system. This gives us new tools in our fight against brain cancer, to essentially correct these deficits and further enhance the ability of the immune system, not only to detect but also to destroy brain tumors,” said Keith L. Black, M.D., director of the Institute, Cedars-Sinai’s Division of Neurosurgery and the Comprehensive Brain Tumor Program.
In an animal study, researchers found that intracranial gliomas – aggressive brain tumors – damage the thymus, the gland responsible for the development and potency of the immune system’s T cells. As the thymus shrinks and its normal structure becomes distorted, many of the thymocytes – the “immature” cells destined to become functional T cells potentially capable of destroying a variety of antigens – undergo a process that weakens and kills them.
Thymocytes are derived from bone marrow and as they travel through the thymus they go through a natural selection process that removes the weakest and prepares the strongest to become lymphocytes that can later adapt as needed to meet a variety of immune challenges. When an intracranial glioma is present, the researchers found, the number of healthy T cells leaving the thymus is dramatically reduced, preventing a large-scale attack on the tumor.
Changes to the thymus and “recent thymic emigrant” (RTE) T cells are similar to those seen in advanced cases of AIDS, in which HIV causes thymocyte death. In glioma progression, researchers believe glucocorticoids, hormones produced by the adrenal glands, are involved in the loss of thymocytes.
The authors noted that physical stress on the body may play a significant role because it causes the release of glucocorticoids. In rats that had their adrenal glands removed to reduce the production of glucocorticoids, the damaging effects were significantly less pronounced.
This finding may also have implications for the way physicians currently treat swelling of brain tissue in patients who have brain tumors. Synthetic glucocorticoids administered to reduce intracranial pressure are highly effective for this purpose but their impact on the thymus and T cells may be further inhibiting an already embattled immune system.
Although CD8(+) cells are produced elsewhere in the body, those originating in the thymus appear to have special relevance in anti-glioma immunity, according to the study.
“It appears that these recent thymic emigrant T cells preferentially home to gliomas or they have an enhanced anti-tumor activity that allows them to home there preferentially,” said Christopher J. Wheeler, Ph.D., research scientist and corresponding author on both papers.
“In a sense, we see two mechanisms working against each other,” said Dr. Wheeler, “Recent thymic emigrant T cells are homing to the tumor, but there is a subversion of thymic function by the tumor itself. Therefore, while we have those cells preferentially homing – they’re enriched relative to other cells – we don’t have a lot of those cells to begin with.”
According to the second paper, the tumor’s immediate environment also changes in a way that thwarts an effective tumor-infiltrating response.
The population of “types” of T cells found in aggressive, malignant tumors was out of balance compared to the response seen in benign tumors. Benign tumors had a high proportion of CD8(+) T cells compared to CD4(+) T cells, which is an indication of a strong tumor-killing immune response. In contrast, nearly all gliomas exhibited greater proportions of CD4(+) relative to CD8(+) T cells.
This manipulation of tumor-infiltrating lymphocytes does not appear to be controlled by the tumor cells themselves but at least to some extent by properties of surrounding tissue, and the ratio correlated directly with the involvement of specific protein molecules detected in nearby cells.
The suspect proteins, Fas ligand (FasL) and Fas, exist in normal brain and blood vessel lining tissue and play a role in immune system regulation. Based on this study, however, they also are expressed on tumor-associated endothelial cells where they may intercept the cancer-fighting T lymphocytes. Endothelial cells make up the lining of blood vessels.
According to the article, increasing levels of endothelial FasL correlated with decreasing proportions of tumor-infiltrating cytotoxic T lymphocytes – tumor-killing immune cells. This suggests the possibility that Fas ligand contributes to a tumor’s ability to evade the immune system.
Taken together, the studies indicate that malignant brain tumors are protected against immunity because the number of potential T cells is reduced in the thymus, and those that initially survive may later be damaged or destroyed.
Malignant gliomas continue to be considered incurable with a short length of survival, although researchers at the Institute have devised a vaccine strategy that has provided encouraging results in early trials. The treatment, called dendritic cell immunotherapy, assists the immune system in recognizing cancer cells as targets for attack, but it depends on the existence of healthy T cells to launch and sustain the immune response.
“The immune system will try to fight off a malignant brain tumor but because it does not accomplish this very effectively, we’re trying to enhance its ability with our cancer vaccine and other therapies,” said Dr. Black, who holds Cedars-Sinai’s Ruth and Lawrence Harvey Chair in Neuroscience.
“We know that the strongest predictor of survival in patients with brain tumors is age. The younger immune system is better able to put up resistance than an older immune system because the thymus naturally becomes weaker and it has fewer precursors of immune cells to recruit in the fight against the tumor. We observe a strong correlation between the survival of a tumor and patient age, which is directly proportional to the number of T cells produced by the thymus.”
The current studies provide insights that may lead to methods to prevent loss of T cells, repair those that become damaged, and strengthen and replenish the supply needed to contain and destroy brain tumors.
Media Contact
More Information:
http://www.csmc.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
Silicon Carbide Innovation Alliance to drive industrial-scale semiconductor work
Known for its ability to withstand extreme environments and high voltages, silicon carbide (SiC) is a semiconducting material made up of silicon and carbon atoms arranged into crystals that is…
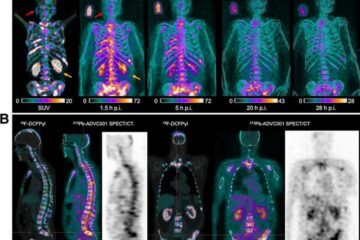
New SPECT/CT technique shows impressive biomarker identification
…offers increased access for prostate cancer patients. A novel SPECT/CT acquisition method can accurately detect radiopharmaceutical biodistribution in a convenient manner for prostate cancer patients, opening the door for more…

How 3D printers can give robots a soft touch
Soft skin coverings and touch sensors have emerged as a promising feature for robots that are both safer and more intuitive for human interaction, but they are expensive and difficult…





















