Unique Test Enables Specialists to Predict Response to Therapy that Makes Poor Donor Matches Compatible

A year-and-a-half after graduating from college in 1999, the last thing that Steve Smith, now 25, expected was for his kidneys to fail. Although the Nashville resident had always been active and healthy and had no family history of kidney disease, shortly after moving to Los Angeles, he began experiencing what he describes as “strange symptoms” that he thought might be associated with mononucleosis. When he went to the doctor, he learned that his kidneys had failed.
He moved back to Nashville and received his first kidney transplant in May, 2000, but his body developed high antibodies and rejected the organ seven months later. Worse still, because of the high antibodies, it was unlikely that doctors would be able to find another match for him as his body would very likely see another donor kidney as a foreign intruder and reject it.
However, neither Smith nor his physicians were willing to give up. His doctors had heard of an innovative kidney transplant therapy that was developed at Cedars-Sinai Medical Center in Los Angeles. They told Smith about it, and he went online to do additional research. He learned that the therapy, known as intravenous immunoglobulin (IVIG) makes kidney transplantation possible between donors and recipients who previously would have been considered poor matches. Smith learned that a new test could help determine which patients were most likely to benefit.
IVIG therapy, which has been used for several years for other diseases, was adapted for use in the field of transplantation by researchers led by Stanley C. Jordan, M.D., medical director of Cedars-Sinai’s Kidney Transplant Program, director of Pediatric Nephrology and Transplant Immunology, and professor of pediatrics at the University of California, Los Angeles. In September, 2002, Smith traveled to Los Angeles where he was seen by Dr. Jordan.
After successfully undergoing the new test to determine whether the IVIG therapy would prove effective for Smith, his donor-friend also flew to Los Angeles for additional testing. The results showed that the therapy would likely be effective in Smith’s case, so the transplant was scheduled for a couple of weeks later.
Prior to the transplant, Smith received two, four-hour treatments of IVIG therapy – an intravenous drip while he was on dialysis. About a month after his transplant, he received a final treatment with IVIG.
“I feel good!” he says now. “The blood test scores are great. I just took my donor on a cruise and I’m trying to get my life back on track.”
Just a few years ago, Smith would have been facing a lifetime of kidney dialysis and little hope for a transplant. Thanks to these new medical advances, though, he has moved back to Los Angeles to resume his career in the entertainment industry.
Coming at a time when the waiting list for cadaveric kidneys is predicted to climb to 100,000 patients by 2006 and 150,000 by 2010, these new techniques may result in greater access to transplantation for many patients who otherwise would have had little hope. In fact, a study published by Dr. Jordan in the American Journal of Transplantation in 2002, showed that the procedure appears to dramatically increase success for patients receiving cadaver organs as well as those receiving kidneys from living relatives or friends.
The infusion of IVIG has been used for several years to help prevent rejection, even in difficult cases when other anti-rejection methods have failed. While most anti-rejection medications suppress the immune system entirely, thereby increasing the patient’s risk of infection, IVIG appears to control immune responses that would harm a transplanted organ, while boosting protection from infection.
Dr. Jordan and his team have now fine-tuned their techniques in the laboratory to predict which patients would most likely benefit from IVIG. By introducing IVIG into the analysis, they are able to make poor matches much more compatible.
The process of “crossmatching” is performed by combining a sample of the potential recipient’s blood serum with a sample of the potential donor’s white cells. The question of compatibility revolves around human leukocyte antigen (HLA), proteins that regulate the way the body recognizes foreign substances.
If the recipient has developed antibodies to the donor’s HLA, the antibody attacks the antigen as an invader. This is called a “positive” crossmatch and it indicates that the recipient’s immune system would reject the donor’s organ. The potential recipient is said to be “sensitized” to the donor’s HLA. If the recipient does not have antibodies against the donor’s HLA – a negative crossmatch – this reaction does not occur.
Because highly sensitized patients have comparatively high risks of rejection and low organ-survival success rates, transplants for these patients have decreased drastically in the past 15 years. Further, there have been no therapies available to resolve issues of immune incompatibility, leaving most patients to rely on dialysis for extended periods of time in the hope that a well-matched kidney might become available.
But Dr. Jordan and his colleagues showed that adding IVIG during the crossmatch process in the laboratory inhibited the destruction of incompatible HLA-bearing cells, in most cases, essentially changing a positive crossmatch to a negative one. Subsequently, patients were able to receive IVIG therapy and undergo a transplant, if the crossmatch became negative after IVIG treatment.
“Based on our results, the IVIG crossmatch technique is a very effective predictor of the way IVIG will help a patient’s immune system to accept a transplanted organ,” said Dr. Jordan. “Those who have a good response in the laboratory can be given IVIG, which eliminates the positive crossmatch and allows for successful transplantation, in most cases. Therefore, a positive crossmatch does not necessarily mean that a patient cannot receive a transplant.”
Cedars-Sinai Medical Center is one of the largest nonprofit academic medical centers in the Western United States. For the fifth straight two-year period, it has been named Southern California’s gold standard in health care in an independent survey. Cedars-Sinai is internationally renowned for its diagnostic and treatment capabilities and its broad spectrum of programs and services, as well as breakthroughs in biomedical research and superlative medical education. Named one of the 100 “Most Wired” hospitals in health care in 2001, the Medical Center ranks among the top 10 non-university hospitals in the nation for its research activities.
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
High-energy-density aqueous battery based on halogen multi-electron transfer
Traditional non-aqueous lithium-ion batteries have a high energy density, but their safety is compromised due to the flammable organic electrolytes they utilize. Aqueous batteries use water as the solvent for…

First-ever combined heart pump and pig kidney transplant
…gives new hope to patient with terminal illness. Surgeons at NYU Langone Health performed the first-ever combined mechanical heart pump and gene-edited pig kidney transplant surgery in a 54-year-old woman…
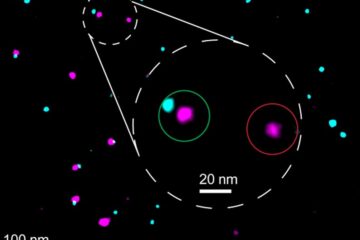
Biophysics: Testing how well biomarkers work
LMU researchers have developed a method to determine how reliably target proteins can be labeled using super-resolution fluorescence microscopy. Modern microscopy techniques make it possible to examine the inner workings…





















