Prenatal stem cell transplants may open door to organ transplants, treating genetic diseases

In a finding that could open the door to future treatments for many genetic diseases such as sickle cell anemia and muscular dystrophy, researchers have produced high levels of transplanted, healthy stem cells in mice, while sharply reducing a hazardous side effect of cell and organ transplants called graft-versus-host disease.
By combining prenatal transplants of blood-forming stem cells with manipulations of blood cells after birth, researchers at The Children’s Hospital of Philadelphia achieved immune tolerance in mice, allowing donor cells to multiply without toxic side effects. The studies appear in related articles in the August and September issues of Blood.
The finding could greatly broaden the use of cell and organ transplants for genetic diseases detected before birth, such as leukemia, sickle cell disease, muscular dystrophy, and some kidney and liver disorders.
“Recent developments in genetic knowledge and technology are converging to make it likely that within a decade, nearly all human genetic diseases will be diagnosed before birth,” says Alan W. Flake, M.D., director of the Children’s Institute for Surgical Science at The Children’s Hospital of Philadelphia, and senior author of both articles. “Our research may greatly expand our ability to use prenatal interventions to help the body safely tolerate treatments for genetic diseases.”
Dr. Flake’s team used a prenatal procedure called in utero hematopoietic stem cell transplantation (IUHSCT). Hematopoietic stem cells develop into red blood cells, white blood cells and a variety of immune cells. The stem cells used in these studies were taken from the bone marrow of adult mice, not from human embryos.
As a disease treatment, prenatal stem cell transplants have faced a major barrier in that they have been unable to achieve high levels of engraftment – the number of donor stem cells usually does not grow large enough to overcome the effect of diseased cells. An exception to this limitation is diseases in which donor cells have a normal advantage over the transplant recipient’s cells. For instance, Dr. Flake was able to cure a child of a rare immune disease, X-linked severe combined immunodeficiency disorder (X-SCID), by using a prenatal stem cell transplant in 1996 that rebuilt his immune system.
Dr. Flake’s current studies potentially extend prenatal stem cell transplants to a broader range of diseases, by manipulating conditions to create a competitive advantage for donor cells over host cells. The IUHSCT procedure first makes the recipient’s immune system tolerant of low levels of donor cells, and then a second, nontoxic procedure after birth provides a competitive advantage for the transplanted donor cells, allowing them to multiply.
“Performing the stem cell transplant prenatally relies on features of the fetal immune system that are more receptive to transplantation,” said Dr. Flake. “For instance, the immaturity of the fetal immune system makes it less able to mount an immune response against the transplanted cells.” Paradoxically, the technique also relies on a strength of the fetal immune system: its healthy thymus, a gland that declines in function after puberty. The fetal thymus produces T-regulatory cells, which help to reduce graft-versus-host disease. In that disease, a life-threatening complication of cell and organ transplants, donor cells attack the patient’s tissues.
The second, postnatal step of the treatment compromises host blood cells and allows the donor cells to engraft themselves in the recipient’s bone marrow and bloodstream. Because the prenatal transplant has made the host animal tolerant of donor cells, the postnatal procedure can be less toxic than conventional treatments that use harsh chemotherapy drugs or high-dose radiation to wipe out the host’s existing immune system.
In one study, Dr. Flake used donor lymphocyte infusion (DLI) as the postnatal treatment. Currently used against some leukemias, DLI supplies lymphocytes, donated immune cells that weaken or kill host blood cells. In the other study, the postnatal treatment was low-dose full-body irradiation followed by bone marrow transplantation. Graft-versus-host disease was minimal in the DLI study, killing only one mouse out of 56, and did not occur at all in the other study.
The procedures achieved complete or near-complete chimerism – meaning that all, or nearly all, of the animal’s blood cells were derived from the donor stem cells, even though the donor animals were not matched with the recipients. “This was the first time that complete chimerism was achieved across mismatched donors and recipients without using toxic therapy,” said Dr. Flake. “If this strategy can be made to work in people, there are broad implications for treating human disease.”
Potential applications to disease treatment
“This approach could potentially target any diseases that are now treatable with bone marrow transplants,” adds Dr. Flake. “These include blood cell diseases such as leukemias, thalassemia and sickle cell disease, as well as many inherited immunodeficiency disorders.”
Beyond that, he added, the technique might also treat muscular dystrophy, an incurable genetic disease that impairs muscle development. In previous research, Dr. Flake’s team showed that stem cells transplanted in utero can develop into healthy muscle cells in mice with muscular dystrophy.
Organ transplant recipients might also benefit from the technique’s ability to make a patient’s immune system tolerant of the donated organ. “If prenatal screening predicts that a fetus would have kidney or liver failure, the prenatal stem cell transplant could prepare the immune system for a future transplant,” says Dr. Flake. “A tolerized immune system would better accept an organ transplant from an unmatched donor.”
Although prenatal screening is not yet widespread for many genetic diseases, he adds, currently emerging technologies will make it feasible to diagnose nearly all genetic diseases early in gestation within the next 10 years. “The combination of data from the Human Genome Project, improvements in molecular diagnoses, gene chip technology, and the ability to do molecular diagnoses of fetal cells or fetal DNA within the mother’s blood, all support early gestational diagnosis of genetic disease,” says Dr. Flake.
Dr. Flake cautions that the clinical applications may be years away, but based on these results, he will further investigate stem cell transplantation in mice and then in larger animals, with the goal of translating the approach to treatments for people.
Media Contact
More Information:
http://www.chop.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
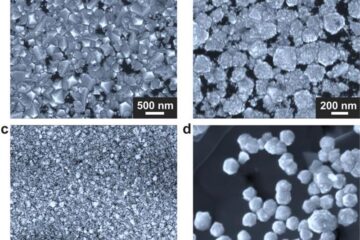
Making diamonds at ambient pressure
Scientists develop novel liquid metal alloy system to synthesize diamond under moderate conditions. Did you know that 99% of synthetic diamonds are currently produced using high-pressure and high-temperature (HPHT) methods?[2]…
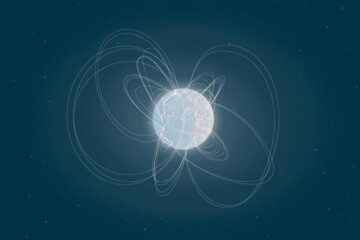
Eruption of mega-magnetic star lights up nearby galaxy
Thanks to ESA satellites, an international team including UNIGE researchers has detected a giant eruption coming from a magnetar, an extremely magnetic neutron star. While ESA’s satellite INTEGRAL was observing…
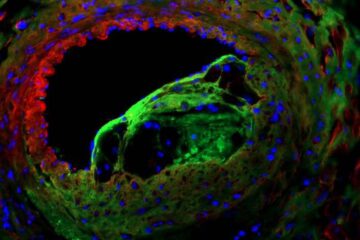
Solving the riddle of the sphingolipids in coronary artery disease
Weill Cornell Medicine investigators have uncovered a way to unleash in blood vessels the protective effects of a type of fat-related molecule known as a sphingolipid, suggesting a promising new…





















