High blood pressure: only one number matters for patients over 50

The proposal is put forward by three hypertension experts in a Viewpoint published early Online and in an upcoming edition of The Lancet. All three experts are attending this week’s International Society of Hypertension meeting in Berlin.
Systolic blood pressure (SBP) is the peak pressure in the arteries at the beginning of the heart’s pumping cycle, while diastolic blood pressure (DBP) is the lowest pressure in the rest phase of the cycle. Both are routinely measured in patients, to give a value of systolic over diastolic, eg. 120/80 mm Hg.
Bryan Williams, University of Leicester and Leicester Royal Infirmary, UK, Lars H. Lindholm, Umeå University Hospital, Sweden, and Peter Sever, International Centre for Circulatory Health, Imperial College London, UK, say that, because of aging populations, systolic hypertension (SH) is becoming much more common and important due to its high prevalence in patients over 50, compared with diastolic hypertension (DH).
SBP rises with age; but DBP only rises until age 50 years and falls thereafter, at a time when risk of cardiovascular disease begins to rise. Thus there is an increased prevalence of SH over age 50 years and an almost total disappearance of DH. The authors say: “Since more than 75% of people with hypertension are aged over 50 years, the burden of disease in mainly due to systolic pressure. The use of diastolic pressure for diagnosis and risk analysis in our ageing populations has thus become illogical.”
In order to simplify treatment strategies for physicians and policy makers, as well as to better focus the minds of drug innovators on the correct targets, the authors propose that, in patients over 50, only SBP needs to be measured, for four reasons. Firstly, SBP is more easily and accurately measured than DBP and is a better predictor of risk. Second, communication with patients would be much easier with just one number, ie, their SBP, since two different numbers leave many of them confused about which is of greater significance. Third, doctors themselves have received many conflicting messages about SBP and DBP, and many still use DBP to guide treatment decisions. This proposal would simplify things for them. And lastly, focussing a public-health campaign on a single number for people aged over 50 years has the potential to dramatically improve treatment outcomes for those with SH, and reduce the associated disease and death rates.
The risk of cardiovascular disease rises continuously as SBP increases from 115 mm Hg. Most international and national guidelines advocate a target of below 140 mm Hg, but there is a lack of evidence from prospective randomised clinical trials to define the best target for SBP treatment. The authors say: “Such trials are much needed and perhaps our call for a renewed focus on SBP will provide a catalyst for them to be designed.”
The authors acknowledge that for patients aged under 50 years, the scenario is different. In patients aged under 40 years, up to 40% of patients with hypertension have isolated DH, while between 40 and 50 years this figure is around a third. Thus for these patients, a continued emphasis on both SBP and DBP is appropriate. The authors say: “However, this much smaller group of patients should not dilute the key message regarding the overwhelming importance of systolic blood pressure for most patients with hypertension.” They add that focussing on SBP in these younger patients will almost always result in adequate control of DBP; yet if DBP is the sole target, many patients most at risk will be left with uncontrolled SPB.
They conclude: “We believe that systolic blood pressure should become the sole defining feature of hypertension and key treatment target for people over age 50 years…[this] will simplify the message for practitioners and for patients, will improve awareness and understanding of treatment objectives, and will ultimately lead to more effective treatment of high blood pressure. Such an initiative would have major public-health implications for the prevention of blood-pressure related cardiovascular disease.”
Media Contact
More Information:
http://www.leicester.ac.ukAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Bringing bio-inspired robots to life
Nebraska researcher Eric Markvicka gets NSF CAREER Award to pursue manufacture of novel materials for soft robotics and stretchable electronics. Engineers are increasingly eager to develop robots that mimic the…

Bella moths use poison to attract mates
Scientists are closer to finding out how. Pyrrolizidine alkaloids are as bitter and toxic as they are hard to pronounce. They’re produced by several different types of plants and are…
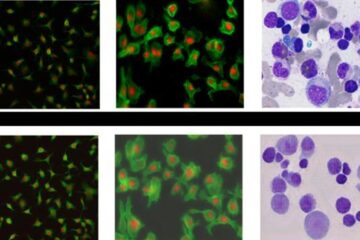
AI tool creates ‘synthetic’ images of cells
…for enhanced microscopy analysis. Observing individual cells through microscopes can reveal a range of important cell biological phenomena that frequently play a role in human diseases, but the process of…





















