Comparison of Venlafaxine and SSRIs in the Treatment of Depression

A new study published in the February 15th issue of Biological Psychiatry set out to compare two popular classes of antidepressants, the newer serotonin and norepinephrine reuptake inhibitors (SNRIs), like venlafaxine (Effexor), and the older selective serotonin reuptake inhibitors (SSRIs), like fluoxetine (Prozac) and citalopram (Celexa), to determine if one provides an overall greater benefit.
To do so, the authors performed a meta-analysis, by pooling the results of 34 double-blind randomized controlled trials that compared a single SNRI, venlafaxine, to other SSRIs. Dr. Charles Nemeroff, senior author on the paper, reports their findings: “Venlafaxine was superior to SSRIs in efficacy overall, and moreover, statistically superior to fluoxetine but not to paroxetine, sertraline or citalopram. Venlafaxine had a higher dropout rate due to adverse events.” These findings indicated a 5.9% advantage in remission rates for venlafaxine. The authors also report that the typical doctor would need to treat 17 patients to have a single patient benefit from being treated with venlafaxine rather than an SSRI.
Acknowledging the seemingly small advantage, John H. Krystal, M.D., Editor of Biological Psychiatry and affiliated with both Yale University School of Medicine and the VA Connecticut Healthcare System, comments that this article “highlights an advance that may have more importance for public health than for individual doctors and patients.” He explains this reasoning:
If the average doctor was actively treating 200 symptomatic depressed patients and switched all of them to venlafaxine from SSRI, only 12 patients would be predicted to benefit from the switch. This signal of benefit might be very hard for that doctor to detect. But imagine that the entire population of depressed patients in the United States, estimated to be 7.1% of the population or over 21 million people, received a treatment that was 5.9% more effective, then it is conceivable that more than 1 million people would respond to venlafaxine who would not have responded to an SSRI. This may be an example of where optimal use of existing medications may improve public health even when it might not make much difference for individual doctors and patients.
Thus, in the typical clinical practice this difference constitutes a barely detectable benefit, but this difference could be meaningful across the large population of depressed patients in the United States.
Media Contact
More Information:
http://www.elsevier.com/All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Superradiant atoms could push the boundaries of how precisely time can be measured
Superradiant atoms can help us measure time more precisely than ever. In a new study, researchers from the University of Copenhagen present a new method for measuring the time interval,…
Ion thermoelectric conversion devices for near room temperature
The electrode sheet of the thermoelectric device consists of ionic hydrogel, which is sandwiched between the electrodes to form, and the Prussian blue on the electrode undergoes a redox reaction…
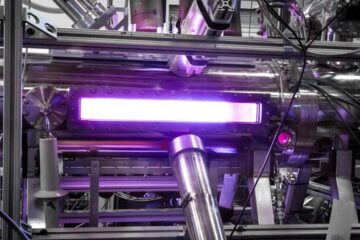
Zap Energy achieves 37-million-degree temperatures in a compact device
New publication reports record electron temperatures for a small-scale, sheared-flow-stabilized Z-pinch fusion device. In the nine decades since humans first produced fusion reactions, only a few fusion technologies have demonstrated…





















