Penn Medicine Researchers Harness the Immune System to Fight Pancreatic Cancer

Pancreatic cancer ranks as the fourth-leading cause of cancer death in the United States, and is one of the most deadly forms of cancer, due to its resistance to standard treatments with chemotherapy and radiation therapy and frequently, its late stage at the time of diagnosis.
A group of researchers led by the University of Pennsylvania’s Perelman School of Medicine and Abramson Cancer Center, in collaboration with scientists from the University of Pittsburgh and University of Washington, published results of a clinical trial in which the standard chemotherapy drug for this disease, gemcitabine, was paired with an agonist CD40 antibody, resulting in substantial tumor regressions among some patients with advanced pancreatic cancer.
By using a novel, real-time imaging approach to monitor tumor response to the immunotherapy, the team also found differences how primary and metastatic disease sites shrank. Their work appears online this month in Clinical Cancer Research.
“We're now using imaging to understand the treatment heterogeneity that one can see in immunotherapy – not all tumors within a patient’s body react the same way, even in the face of powerful treatments, and now we have a way to follow these unique treatment responses in patients in real-time,” said lead author Gregory Beatty, MD, PhD, an assistant professor in the division of Hematology/Oncology in the Abramson Cancer Center.
The report builds on preliminary results of findings in both humans and mice published in Science in 2011. The new approach exploits an immune reaction in the microenvironment of the patient’s primary tumor by targeting an immune cell surface molecule CD40 to turn a type of white blood cell known as macrophages against the tumor by causing them to attack the stroma, the fibrotic supporting tissue of the tumor that acts as a defensive barrier to standard therapies. The treatment ate away at this stroma, ultimately causing substantial shrinkage of some primary tumors, and affecting the metabolic activity of both primary and metastatic lesions. Of 21 patients treated with the drug combination, five patients who received at least one treatment course developed a partial response, defined as a decrease in tumor size of at least 30 percent.
The new study also measured the effectiveness of applying a new approach to FDG/PET-CT imaging, to reveal the metabolic responses of individual tumors. FDG/PET-CT uses a radioactive glucose tracer to pinpoint glucose uptake within tumors, revealing the places where cells are metabolically active. Typically physicians and radiologists report only the maximum uptake of glucose within a tumor using this imaging technique; however, the new study showed that glucose metabolism can be quantified within individual tumors or within organs, and throughout the entire body, to provide a measure of total tumor burden.
The team found that while primary tumors seemed to respond more or less uniformly with each treatment cycle, tumors varied in their reactions to treatment. “We incorporated imaging as early as two weeks after the first dose of treatment, and we're able to see changes and responses in terms of glucose metabolism even at this early time point in treatment, which predicted how well patients would respond two months later,” Beatty says. The team hopes to apply the use of FDG/PET-CT to monitoring treatment responses during other immune-based therapies in pancreas cancer.
Determining the reasons for these varying responses will be an important next step in this work. The unique imaging approach, Beatty notes, is revealing new insight into the biology of pancreas cancer and its treatment resistance. This allows the research team to expedite progress through a unique model that moves quickly back and forth between the lab and the clinic: “We're taking it back to the bench and at the same time, applying it at the bedside with additional clinical trials.”
The most commonly observed side effect of the treatment was cytokine release syndrome, typically manifested as chills and rigors. One patient with a previous history of vascular disease experienced a stroke shortly after starting therapy.
The trial was supported by Pfizer Corporation, with partial funding from the American Society of Clinical Oncology Young Investigator Award and by the National Cancer Institute (CA138907-02, CA169123).
Penn Medicine is one of the world's leading academic medical centers, dedicated to the related missions of medical education, biomedical research, and excellence in patient care. Penn Medicine consists of the Raymond and Ruth Perelman School of Medicine at the University of Pennsylvania (founded in 1765 as the nation's first medical school) and the University of Pennsylvania Health System, which together form a $4.3 billion enterprise.
The Perelman School of Medicine has been ranked among the top five medical schools in the United States for the past 16 years, according to U.S. News & World Report's survey of research-oriented medical schools. The School is consistently among the nation's top recipients of funding from the National Institutes of Health, with $398 million awarded in the 2012 fiscal year.
The University of Pennsylvania Health System's patient care facilities include: The Hospital of the University of Pennsylvania — recognized as one of the nation's top “Honor Roll” hospitals by U.S. News & World Report; Penn Presbyterian Medical Center; Chester County Hospital; Penn Wissahickon Hospice; and Pennsylvania Hospital — the nation's first hospital, founded in 1751. Additional affiliated inpatient care facilities and services throughout the Philadelphia region include Chestnut Hill Hospital and Good Shepherd Penn Partners, a partnership between Good Shepherd Rehabilitation Network and Penn Medicine.
Penn Medicine is committed to improving lives and health through a variety of community-based programs and activities. In fiscal year 2012, Penn Medicine provided $827 million to benefit our community.
Media Contact
More Information:
http://www.uphs.upenn.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Combatting disruptive ‘noise’ in quantum communication
In a significant milestone for quantum communication technology, an experiment has demonstrated how networks can be leveraged to combat disruptive ‘noise’ in quantum communications. The international effort led by researchers…
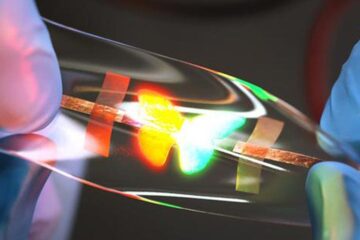
Stretchable quantum dot display
Intrinsically stretchable quantum dot-based light-emitting diodes achieved record-breaking performance. A team of South Korean scientists led by Professor KIM Dae-Hyeong of the Center for Nanoparticle Research within the Institute for…

Internet can achieve quantum speed with light saved as sound
Researchers at the University of Copenhagen’s Niels Bohr Institute have developed a new way to create quantum memory: A small drum can store data sent with light in its sonic…





















