Pain drug can kill resistant tuberculosis

An off-patent anti-inflammatory drug that costs around two cents for a daily dose in developing countries has been found by researchers at Weill Cornell Medical College to kill both replicating and non-replicating drug resistant tuberculosis in the laboratory — a feat few currently approved TB drugs can do, and resistance to those is spreading.
Their findings, published online by the journal PNAS, point to a potential new therapy for the more than 500,000 people worldwide whose TB has become resistant to standard drug treatments. But the researchers worry that the effective drug, oxyphenbutazone, may never be tested in TB clinical trials.
Weill Cornell's Dr. Carl Nathan and his research team found what they call the “completely surprising” ability of oxyphenbutazone to kill drug resistant TB after testing thousands of approved drugs against the bacteria. This repurposing of agents already on the market can lead to quicker testing for new uses.
“This agent might help save lives if there was a way to test it in TB patients,” says Dr. Nathan. Oxyphenbutazone went on the market as a patented drug for arthritis-like pain in the early 1950s, and lost its patent and market dominance by the 1970s.
“It is difficult today to launch clinical studies on a medication that is so outdated in the United States, that it is mainly used here in veterinary medicine to ease pain,” says the study's senior author, Dr. Nathan, chairman of the Department of Microbiology and Immunology, the R.A. Rees Pritchett Professor of Microbiology, and the director of The Abby and Howard Milstein Program in the Chemical Biology of Infectious Disease at Weill Cornell. “No drug firm will pay for clinical trials if they don't expect to make a profit on the agent. And that would be the case for an off-patent drug that people can buy over the counter for pain in most of the world.”
He adds that oxyphenbutazone, best known under the trademark name of Tandearil, does have some established toxicities, “and is not a drug you should take for aches and pains if a safer alternative is available.” But the drug's major toxicities appear to be less frequent than the major side-effects of the drug regimens that are currently used to treat TB, he says.
Treating the TB that Hides
Mycobacterium tuberculosis is unusual among disease-causing bacteria in that it naturally infects just humans. One-third of the world's population is infected with TB, but the bacteria typically remain dormant in a person with a healthy immune system.
Nonetheless, TB becomes active in enough people that it is the leading cause of death in humans from a bacterial infection. It is difficult to treat, and the bacteria can become resistant to therapy. TB treatment in a drug-sensitive patient takes six months, using a combination of agents. If the TB is sensitive to these first-line agents and the therapy is completed with full-strength, non-counterfeit drugs, up to 95 percent of patients can be cured.
However, if a patient's TB becomes resistant to these drugs, second-line agents are administered every day for two years or more. “These second-line drugs are often toxic and expensive, and are not readily available in developing countries, where most of the infections occur,” Dr. Nathan says. Mortality in drug resistant TB patients can be as high as 80 percent.
A major issue in treating TB is that the bacteria can “hide out” in the body in a non-replicating form, even when a TB patient is undergoing treatment.
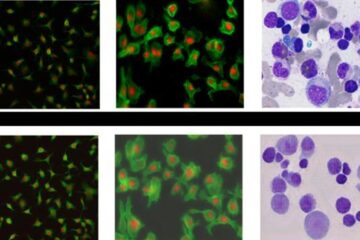
To find agents that could attack non-replicating TB, Dr. Nathan's research team first identified four conditions that keep bacteria in that state within the human body: low oxygen, mild acidity, a fat instead of sugar to eat and a small amount of the natural defense molecule nitric oxide.
The research team replicated those conditions in the test tube and then methodically tested the effectiveness of thousands of agents against the bacteria. After testing 5,600 drugs, researchers found oxyphenbutazone.
Researchers then delved into the mechanism by which oxyphenbutazone kills TB and found that the conditions that allow the bacterium to remain dormant modify the drug to the point that it starts reacting against both non-replicating and replicating TB. “When this happens, TB can't defend itself and dies,” Dr. Nathan says.
But the researchers were unable to test oxyphenbutazone in mice, because the animals metabolize the drug to an inactive form far faster than humans.
“This makes testing the drug for TB use in humans problematic since the FDA requires preclinical animal testing studies for safety and efficacy,” Dr. Nathan says. “Yet there is a long track record of oxyphenbutazone's relatively safe use in hundreds of thousands of people over decades.”
Dr. Nathan and his team are continuing their research, testing hundreds of thousands of compounds for their action against TB. His team has already found another approved drug, nitazoxanide, to be effective against the bacteria, publishing his findings in 2009.
Nitazoxanide, a drug with an excellent safety record, is still on patent for use against some infections caused by other microbes. Discussions have been held about testing it in TB, Dr. Nathan says, but have stalled because of the same problem as oxyphenbutazone. The drug is metabolized so quickly in mice that it cannot be tested against experimental TB in that species.
For both oxyphenbutazone and nitazoxanide, Dr. Nathan argues that the requirement for testing in animals with experimental TB should be waived, because these agents work against TB in the test tube, have already been used with relative safety in people and might address an urgent need for treatment of a contagious disease with high mortality and few other treatment options.
This research was supported by the Tuberculosis Drug Accelerator Program of the Bill and Melinda Gates Foundation and the Abby and Howard P. Milstein Program in Chemical Biology of Infectious Disease.
Co-authors of the study include: Dr. Ben Gold, Dr. Maneesh Pingle, Julia Roberts, Dr. Mark Rundell, Dr. Thulasi Warrier, Dr. Aditya Venugopal, Dr. Crystal Darby, Xiuju Jiang, Dr. J. David Warren, Amy Cunningham-Bussel, Poonam Rath, Tamutenda Chidawanyika, Dr. Selin Somersan and Dr. W. Clay Bracken from Weill Cornell; Dr. Steven J. Brickner of S. J. Brickner Consulting; Dr. Ouathek Ouerfelli and Dr. Nilesh Shah from Memorial Sloan–Kettering Cancer Center; Dr. Eric L. Nuermberger from Johns Hopkins Hospital; and Dr. Joseph Fernandez, Ronald Realubit, Dr. J. Fraser Glickman, and Dr. Haiteng Deng from The Rockefeller University.
Weill Cornell Medical College
Weill Cornell Medical College, Cornell University's medical school located in New York City, is committed to excellence in research, teaching, patient care and the advancement of the art and science of medicine, locally, nationally and globally. Physicians and scientists of Weill Cornell Medical College are engaged in cutting-edge research from bench to bedside, aimed at unlocking mysteries of the human body in health and sickness and toward developing new treatments and prevention strategies. In its commitment to global health and education, Weill Cornell has a strong presence in places such as Qatar, Tanzania, Haiti, Brazil, Austria and Turkey. Through the historic Weill Cornell Medical College in Qatar, the Medical College is the first in the U.S. to offer its M.D. degree overseas. Weill Cornell is the birthplace of many medical advances — including the development of the Pap test for cervical cancer, the synthesis of penicillin, the first successful embryo-biopsy pregnancy and birth in the U.S., the first clinical trial of gene therapy for Parkinson's disease, and most recently, the world's first successful use of deep brain stimulation to treat a minimally conscious brain-injured patient. Weill Cornell Medical College is affiliated with NewYork-Presbyterian Hospital, where its faculty provides comprehensive patient care at NewYork-Presbyterian Hospital/Weill Cornell Medical Center. The Medical College is also affiliated with the Methodist Hospital in Houston. For more information, visit weill.cornell.edu.
Media Contact
All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Bringing bio-inspired robots to life
Nebraska researcher Eric Markvicka gets NSF CAREER Award to pursue manufacture of novel materials for soft robotics and stretchable electronics. Engineers are increasingly eager to develop robots that mimic the…

Bella moths use poison to attract mates
Scientists are closer to finding out how. Pyrrolizidine alkaloids are as bitter and toxic as they are hard to pronounce. They’re produced by several different types of plants and are…
AI tool creates ‘synthetic’ images of cells
…for enhanced microscopy analysis. Observing individual cells through microscopes can reveal a range of important cell biological phenomena that frequently play a role in human diseases, but the process of…





















