Nicotine receptors found for the first time in the mouth open the door to new treatments

A research team by scientists in Portugal and the US has found for the first time nicotine receptors in the taste buds. In fact, although most of the toxicity of smoking is linked to other components, it is nicotine that leads to smoking addiction and until now it was believed that this substance had to migrate into the brain – where its specific receptors existed – to provoke its effects.
This new discovery published in the Proceedings of the National Academy of Sciences (PNAS) reveals a second recognition pathway most probably contributing for addiction and suggesting a possible new target for anti-smoking drugs. The added bonus is that on this route the drugs can be applied topically (on the tongue), drastically reducing their side effects. This novel pathway is also shown to activate a brain area that when damaged can lead to instant loss of smoking addiction suggesting that mouth nicotine receptors can play a key role in the whole dependence process.
Tobacco addiction produces devastating health problems including high number of premature deaths in long-term smokers, half of these occurring as early as middle age. Specific problems include cardiovascular diseases and cancer, but also increased risk of infection such as tuberculosis, insulin resistance and diabetes, healing difficulties as well as reproductive problems and can even lead to infertility. Despite this, just in the United States, 45 million adults smoke and even if numbers are slowly diminishing in developed countries, rates continue to increase in developing countries where as much as 40% of the population can smoke. This while we know that, at least in developed countries, a large percentage of these smokers want to give up but is simply incapable of doing it.
This irresistible power of tobacco, or more exactly, of nicotine, resides in its effect on the brain. Smoke inhalation results in nicotine being transported into the lung from where it enters the blood circulation and is carried into the brain. There it binds nicotinic cholinergic receptors (nAChRs) and ultimately leads to the release of “feel good” neurotransmitters, such as dopamine. The problem is that long-term exposure to nicotine leads to an increased number of nicotine receptors in the brain and eventually tolerance to dopamine. This means that when we stop smoking other stimulus are not sufficient to produce enough dopamine to induce sensations of pleasure, and a general state of “unhappiness” – so well known to those trying to stop the habit – occurs. Withdrawal symptoms include restlessness, anxiety, concentration problems and, of course, a constant craving for tobacco.
Other factors such as culture or even habits of association such as “a coffee and a cigarette” contribute to the whole pattern of addiction. Drugs to combat smoke addiction interfere with the nicotine receptors in the brain, while slowly desensitising the individual to dopamine but, not only they carry a multitude of side effects, such as severe depression, but also have reduced success rates with only about 20% of people remaining smoke-free on the long-term. Recently, widespread prohibition of smoking in public spaces was hoped to affect smoking numbers but results, so far, are not very promising highlighting the urgency for new strategies to combat the problem.
It is in this context that Albino J. Oliveira-Maia, Jennifer R. Stapleton-Kotloski, Miguel A. L. Nicolelis, Sidney A. Simon and colleagues at the Medicine Faculty and the Institute of Cellular and Molecular Biology in the University of Porto, Portugal; Virginia Commonwealth University, Virginia, USA; Duke University Medical Center, North Carolina, USA; and the Edmond and Lily Safra International Institute for Neuroscience of Natal, Rio Grande do Norte, Brazil, decided to look into a recently described mouse lacking a protein – called TRPM5 – linked to the recognition of bitter tastes (nicotine is known to be bitter) since previous research have suggested that taste is important for tobacco addiction. In fact individuals with an extreme capacity to taste bitterness are more resistant to smoke addiction, while lesions to the insula – a brain area where the gustatory cortex is localised – can affect smoking addiction.
To the researchers’ surprise, when comparing normal animals against animals lacking TRPM5 in the presence of nicotine and quinine (that also has a bitter taste) solutions, it was discovered that, although incapable of tasting bitter tastes, Trpm5 negative animals could still distinguish nicotine from water and, more surprisingly, also from quinine. These results suggested a second pathway of recognition- which is TRPM5 and taste independent – for nicotine in the mouth.
And in fact, further studies in rats revealed the existence of nicotine receptors in the Taste Receptor Cells and taste nerves of the mouth, which, when triggered by nicotine, activated the gustatory cortex with a very different neural pattern from the one obtained by the recognition of pure bitter taste, like in quinine case. However, when nicotinic cholinergic receptors (nAChRs) inhibitors – used to stop smoking – were put on the tongue, both the behavioural and neural effects of nicotine became similar to those obtained with quinine.
What Oliveira-Maia, Simon and colleagues’ results reveal is that nicotine stimulates two systems in the mouth, one related to TRPM5, which is also used to recognise other bitter substances such as quinine, and a second one apparently specific for nicotine and Trpm5 independent. This last recognition system leads to an unique neural activation pattern of the gustatory cortex probably linked to nicotine addiction. The clue to this resides in the fact that damage in the brain insula area – where the gustatory cortex is – can eliminate any addiction to tobacco even in chronic smokers using several packets a day just before the injury. If the mouth nicotine receptors are confirmed to be linked with these insula effects, blocking them can turn out to be “the” weapon against smoking.
Either way, Oliveira-Maia and colleagues’ discovery raises the possibility of, not only using anti-smoking drugs topically avoiding in this way many of the side effects seen when the drugs are used sistemically, but also, by creating a second front of attack, contributing to more efficient anti-smoking therapies crucial in a world where smoking still kills more than 5 million people a year worldwide.
Piece by Catarina Amorim (catarina.amorim at linacre.ox.ac.uk)
Media Contact
More Information:
http://www.pnas.org/All latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Properties of new materials for microchips
… can now be measured well. Reseachers of Delft University of Technology demonstrated measuring performance properties of ultrathin silicon membranes. Making ever smaller and more powerful chips requires new ultrathin…

Floating solar’s potential
… to support sustainable development by addressing climate, water, and energy goals holistically. A new study published this week in Nature Energy raises the potential for floating solar photovoltaics (FPV)…
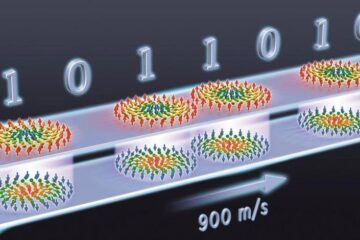
Skyrmions move at record speeds
… a step towards the computing of the future. An international research team led by scientists from the CNRS1 has discovered that the magnetic nanobubbles2 known as skyrmions can be…





















