Light activated treatments could solve MRSA problems after surgery

“We showed that 99% of the potentially dangerous Staphylococcus aureus bacteria in infected wounds can be killed using a green dye that gives off toxic molecules when it is activated by near-infrared light,” said Dr Ghada Omar from University College London, UK.
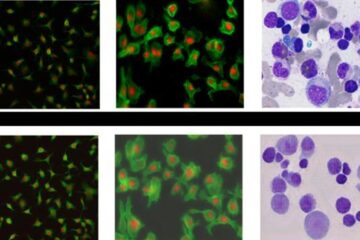
Near-infrared light is commonly used in fibre-optics and telecommunications because it passes through glass easily. Researchers have now discovered that it can be used alongside a dye to kill bacteria that infect wounds and burns. The dye used, called indocyanine green, is harmless to humans and inactive in the dark. However, it gives off toxic molecules that rapidly kill the bacteria when it is triggered by the right light wavelengths.
“The chemicals produced when the dye is activated harm the bacteria in such a wide variety of ways that it is unlikely bacteria could ever develop resistance to the treatment,” said Dr Omar. This makes it ideal – and possibly the only option – for treating infections with multiple drug resistant bacteria, including MRSA.”
Infected wounds are a major problem for thousands of hospital patients every year, and up to 9% of hospital acquired infections occur during surgery, contributing to 77% of deaths from surgical operations. These infections increase the length of time patients must remain in hospital by an average of 10 days, increasing the cost to the NHS by up to two and a half times to as much as £2,400 per patient.
The new light-activated antimicrobial treatment is less effective when there are low oxygen levels in the infected tissues. This is a common problem in injuries where blood systems have been damaged, or where the injury is further away from the bodies' main vascular systems. The latest work from the University College London team shows that even with very low oxygen levels in the damaged tissues, most dangerous bacteria can still be killed using the light-activated dyes.
“Increasing oxygen levels in the infected tissues would maximise the killing effect”, said Dr Omar. “But even with low oxygen levels a very wide range of bacteria were killed, including over 70% of Streptococcus pyogenes and Staphylococcus aureus, which has become one of the most drug resistant bacteria in hospitals.” Dr Omar's co-authors on the study include Michael Wilson and Sean Nair of the Division of Microbial Diseases, UCL Eastman Dental Institute.
The research is part of a programme looking for a simple, rapid and cheap alternative treatment for infected wounds and ulcers that do not respond to conventional antibiotics.
Media Contact
More Information:
http://www.sgm.ac.ukAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Bringing bio-inspired robots to life
Nebraska researcher Eric Markvicka gets NSF CAREER Award to pursue manufacture of novel materials for soft robotics and stretchable electronics. Engineers are increasingly eager to develop robots that mimic the…

Bella moths use poison to attract mates
Scientists are closer to finding out how. Pyrrolizidine alkaloids are as bitter and toxic as they are hard to pronounce. They’re produced by several different types of plants and are…
AI tool creates ‘synthetic’ images of cells
…for enhanced microscopy analysis. Observing individual cells through microscopes can reveal a range of important cell biological phenomena that frequently play a role in human diseases, but the process of…





















