New islet cell transplant procedure offers improved outcomes for patients with type 1 diabetes

The latest approach to islet transplantation, in which clusters of insulin-producing cells known as islets are transplanted from a donor pancreas into another person's liver, has produced substantially improved results for patients with type 1 diabetes, and may offer a more durable alternative to a whole pancreas transplant.
Participants in the new study received islet cells isolated from the pancreas of organ donors to help their bodies produce insulin, the life-sustaining hormone responsible for absorbing glucose from the blood. The new approach, which allowed the harvested cells a short period of rest prior to transplant, resulted in increased levels of insulin production to the degree that patients were able to discontinue daily insulin injections. Results of the study, conducted by researchers at the Perelman School of Medicine at the University of Pennsylvania, appeared recently in the journal Diabetes.
In the study, investigators used an advanced technique to isolate and harvest islet cells from donor pancreases. Unlike prior methods in which isolated islet cells were immediately transferred to the recipient, the new technique allowed the extracted cells to rest in a controlled environment for three days prior to transplant. Inflammation that occurs when the cells are harvested can often predispose the recipient to rejection after transplantation. However, by allowing the cells to rest, the inflammation – and possibility of rejection – is reduced. Ultimately, the resting period also resulted in a more efficient process by allowing investigators to use fewer islet cells than previous methods which required cells from two or more donor pancreases achieve similar results. Despite fewer islet cells being transplanted, the new approach resulted in significantly improved islet cell function.
“These results show that islet transplantation has become a more promising method for replacing the islet cells in type 1 diabetes patients experiencing severe problems with low blood sugar,” said lead author Michael R. Rickels, MD, MS, medical director for the Pancreatic Islet Cell Transplantation Program and associate professor of Medicine in Endocrinology, Diabetes and Metabolism at Penn Medicine. “We've seen positive long-term results with this technique, and are excited to be able to offer the option to our patients, where currently a whole pancreas transplant requiring major surgery is the only available alternative.”
The new approach, known as the CIT07 protocol, was developed by the National Institutes of Health and sponsored by the Clinical Islet Transplantation (CIT) Consortium, in which Penn has served as a member since 2004. Under the new protocol, which measures islet cell mass, all patients involved in the study were able to come off insulin therapy and remained so after at least one year with no loss of the transplanted cell mass.
Typically, patients with type 1 diabetes must self-administer multiple injections of insulin per day, or receive it by a continuous infusion from a wearable pump. However, insulin therapy is difficult to calibrate to the body's changing energy needs, and patients are required to frequently check their blood sugar levels and adjust their insulin dosage. Varying levels of insulin in the body often results in low blood sugar (hypoglycemia), which can induce a coma or other medical emergency. Conversely, islet transplantation, when effective, results in natural, internal self-monitoring and adjustment of insulin levels to keep blood sugar levels in a normal range (homeostasis).
“The fact that significantly more transplanted islet cells in the new protocol are able to successfully integrate and continue producing insulin at least one year later compared to prior studies, gives us hope that more type 1 diabetes patients will be able to live full and healthy lives free from the dangers of hypoglycemia and the burden of administering insulin,” said senior author and principal investigator Ali Naji, MD, PhD, surgical director of the Kidney and Pancreas Transplant Program at Penn Medicine.
Roughly five to ten percent of all people with diabetes have Type 1 diabetes. Previously known as juvenile-onset diabetes, Type 1 diabetes is typically first diagnosed in children and young adults and persists throughout life. Patients with the disease do not produce insulin because of autoimmune destruction of the insulin producing cells in the pancreas. Without insulin, patients cannot convert sugar, starches, and other food into energy needed for survival. When left untreated, Type 1 diabetes is a potentially fatal disease.
Penn Medicine is one of the world's leading academic medical centers, dedicated to the related missions of medical education, biomedical research, and excellence in patient care. Penn Medicine consists of the Raymond and Ruth Perelman School of Medicine at the University of Pennsylvania (founded in 1765 as the nation's first medical school) and the University of Pennsylvania Health System, which together form a $4.3 billion enterprise.
The Perelman School of Medicine has been ranked among the top five medical schools in the United States for the past 16 years, according to U.S. News & World Report's survey of research-oriented medical schools. The School is consistently among the nation's top recipients of funding from the National Institutes of Health, with $398 million awarded in the 2012 fiscal year.
The University of Pennsylvania Health System's patient care facilities include: The Hospital of the University of Pennsylvania — recognized as one of the nation's top “Honor Roll” hospitals by U.S. News & World Report; Penn Presbyterian Medical Center; Chester County Hospital; Penn Wissahickon Hospice; and Pennsylvania Hospital — the nation's first hospital, founded in 1751. Additional affiliated inpatient care facilities and services throughout the Philadelphia region include Chestnut Hill Hospital and Good Shepherd Penn Partners, a partnership between Good Shepherd Rehabilitation Network and Penn Medicine.
Penn Medicine is committed to improving lives and health through a variety of community-based programs and activities. In fiscal year 2012, Penn Medicine provided $827 million to benefit our community.
Media Contact
More Information:
http://www.uphs.upenn.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
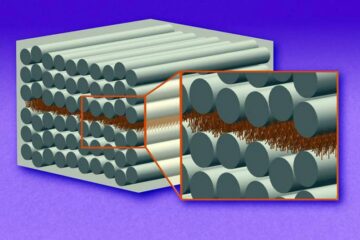
“Nanostitches” enable lighter and tougher composite materials
In research that may lead to next-generation airplanes and spacecraft, MIT engineers used carbon nanotubes to prevent cracking in multilayered composites. To save on fuel and reduce aircraft emissions, engineers…

Trash to treasure
Researchers turn metal waste into catalyst for hydrogen. Scientists have found a way to transform metal waste into a highly efficient catalyst to make hydrogen from water, a discovery that…
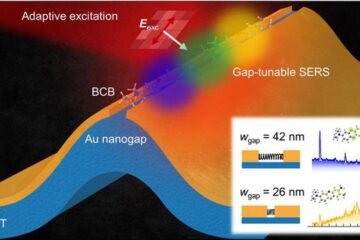
Real-time detection of infectious disease viruses
… by searching for molecular fingerprinting. A research team consisting of Professor Kyoung-Duck Park and Taeyoung Moon and Huitae Joo, PhD candidates, from the Department of Physics at Pohang University…





















