Experimental Alzheimer's disease drugs might help patients with nerve injuries

Drugs already in development to treat Alzheimer's disease may eventually be tapped for a different purpose altogether: re-growing the ends of injured nerves to relieve pain and paralysis. According to a new Johns Hopkins study, experimental compounds originally designed to combat a protein that builds up in Alzheimer's-addled brains appear to make crushed or cut nerve endings grow back significantly faster, a potential boon for those who suffer from neuropathies or traumatic injuries.
The new drugs target a protein known as “ƒÒ-Site amyloid precursor protein cleaving enzyme 1,” or BACE1, which plays a key role in generating the amyloid protein plaques that are thought to gum up normal nerve signaling in the brain. Previous laboratory research showed that BACE1 also is involved in creating the insulation material known as myelin, which coats the projections that nerve cells extend to connect with each other, as well as generating a molecular cascade that causes these projections to degenerate when they're injured.
Based on these earlier findings, assistant professor of neurology Mohamed Farah, Ph.D., professor of neurology John Griffin, M.D., and their colleagues tried blocking the action of BACE1 to analyze the effect on injured axon projections. The researchers started their experiments with mice whose ability to make BACE1 had been genetically knocked out. After these animals' sciatic nerves were cut or crushed, the scientists closely watched what happened as the axons regenerated.
Compared to normal mice that make BACE1, the animals lacking this protein cleaned up the debris around the injury site significantly faster. Since this debris can inhibit regeneration, Farah and his colleagues expected that the axons would re-grow faster. Sure enough, the cut ends of the animals' nerve cells generated more new sprouts, which grew into extensions that reached their targets ¡X muscles or other nerve cells ¡X days faster than the mice that made BACE1.
Hopeful that compounds able to block BACE1 activity would have a similar effect, Farah and Griffin's team worked with two experimental drugs already developed to target Alzheimer's disease (BACE1 inhibitor IV, produced by Calbiochem, and WAY 258131, a Wyeth compound that was synthesized by researchers at Johns Hopkins Brain Science Institute for this study). Mice given either of the two drugs systemically after nerve injuries had a similar increase in re-growth, though less pronounced. This was expected, explains Farah, since the drugs dampen the effect of BACE1 without removing it entirely as in the genetic knockout mice.
The Hopkins researchers said their proof of the principle work, published in the Journal of Neuroscience on April 13, was reason to celebrate. “Anything that speeds nerve re-growth could be enormously helpful to people with nerve injuries caused by a range of injuries and diseases, from diabetic neuropathy to motorcycle accidents,” says Farah.
“After an injury, the environment around nerves and their target tissue sometimes degenerates before the nerves can heal, which kills the chances that the nerve will re-grow,” he explains. “If we can help nerves re-grow faster, we increase the chances that they can reach their target and become healthy again after injury.”
As a next step, the researchers plan to test the experimental compounds in other animal models of nerve injury, including neuropathies and spinal cord injuries.
“BACE1 inhibitors are a major drug target for many drug companies for Alzheimer's,” says Griffin. “Our work may suggest that these drugs could have great utility in a very large clinical population with tremendous unmet need. Validation of our early research in other animal models of nerve injury will set the stage for further clinical investigation.”
Other Johns Hopkins researchers who participated in this study include Bao Han Pan, Ph.D., Paul N. Hoffman, M.D., Ph.D., Dana Ferraris, Ph.D., Takashi Tsukamoto, Ph.D., Thien Nguyen, M.D., Ph.D., Philip C. Wong, Ph.D., Donald L. Price, M.D., and Barbara S. Slusher, Ph.D., M.B.A.
For more information, go to:
http://neuroscience.jhu.edu/JohnGriffin.php
http://www.hopkinsmedicine.org/neurology_neurosurgery
Media Contact
More Information:
http://www.jhmi.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
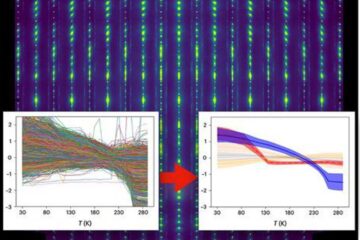
Machine learning algorithm reveals long-theorized glass phase in crystal
Scientists have found evidence of an elusive, glassy phase of matter that emerges when a crystal’s perfect internal pattern is disrupted. X-ray technology and machine learning converge to shed light…
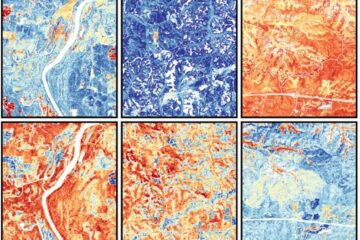
Mapping plant functional diversity from space
HKU ecologists revolutionize ecosystem monitoring with novel field-satellite integration. An international team of researchers, led by Professor Jin WU from the School of Biological Sciences at The University of Hong…

Inverters with constant full load capability
…enable an increase in the performance of electric drives. Overheating components significantly limit the performance of drivetrains in electric vehicles. Inverters in particular are subject to a high thermal load,…





















