Decoding DNA finds breast tumor signatures that predict treatment response

Researchers at Washington University School of Medicine in St. Louis uncovered mutations linked to whether or not women respond to aromatase inhibitors, drugs often prescribed to shrink large tumors before surgery. These mutations also correlate with clinical features of breast tumors, including how likely they are to grow quickly and spread.
The research, which also involved physicians and scientists at the Alvin J. Siteman Cancer Center at Barnes-Jewish Hospital and Washington University School of Medicine and The Genome Institute, is published June 10 in the advance online edition of Nature.
“This is one of the first cancer genomics studies to move beyond cataloging mutations involved in cancer to finding those linked to treatment response and other clinical features,” says senior author Elaine Mardis, PhD, co-director of The Genome Institute. “If our results are validated in larger studies, we think genomic information will be one more data point for physicians to consider when they select among several treatment options for their patients.”
The study involved DNA from 77 post-menopausal women with stage 2 or 3 estrogen-receptor-positive breast cancer, the most common form of the disease. Estrogen stimulates the growth of these tumors, and all the women received aromatase inhibitors to lower estrogen in the body. The drugs can reduce the size of breast tumors, enabling many women to receive breast-conserving surgery rather than a mastectomy. But aromatase inhibitors only work in some women, and doctors don't know why.
To answer that question, the researchers compared the DNA in the tumor samples to matched DNA from the same patients' healthy cells, which allowed them to identify mutations that only occurred in the cancer cells. This “unbiased” approach finds all the mutations underlying a patient's cancer not just those that would be expected to occur.
The tumor samples came from women enrolled in one of two aromatase inhibitor clinical trials sponsored by the American College of Surgeons Oncology Group. As part of those trials, researchers had collected detailed information about the women's tumors and whether they responded to a four-month course of aromatase inhibitor therapy before surgery. Twenty-nine of the tumor samples came from women whose tumors were resistant to aromatase inhibitors, and 48 came from patients whose tumors responded.
Over all, the scientists noted that tumors in women who responded to the estrogen-lowering drugs had relatively few mutations, while those whose cancers were resistant to the treatment had higher mutation rates and were genomically more complex.
“This makes sense in hindsight but it's not something that we would have predicted,” Mardis says.
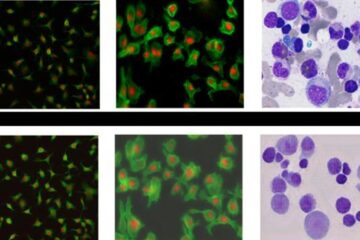
The researchers identified 18 significantly mutated genes in the tumor samples, meaning the genes were altered more often than would have been expected. Some of these genes were already known to be important in breast cancer but others were completely unexpected, including a handful that are well-recognized for their role in leukemia.
To evaluate the clinical significance of the 18 genes, the researchers expanded the study to include an additional 240 women with estrogen-receptor-positive breast cancer whose response to aromatase inhibitor therapy also had been documented.
They found several genes that were relatively common in many of the patients' cancers that also appeared to be linked to treatment response. About 20 percent of women's tumors had mutations in a potent tumor-suppressor gene called TP53. These mutations were linked to a poor response to aromatase inhibitors and to fast-growing tumors that were more likely to metastasize. Women with TP53 mutations also were more likely to have a subtype of breast cancer called luminal B, which has a poor prognosis.
“Rather than give aromatase inhibitors to women with TP53 mutations knowing they are unlikely to be effective, these women may benefit from immediate surgery followed by chemotherapy,” says lead author Matthew Ellis, MD, PhD, the Anheuser Busch Professor of Medical Oncology, who treats patients at the Siteman Cancer Center and Barnes-Jewish Hospital.
In contrast, mutations in MAP3K1 and its “sister” gene MAP2K4 occurred in about 16 percent of patients and were linked to a good response to aromatase inhibitors. Women with mutations in these genes were more likely to have slow-growing tumors that did not spread, and they typically had luminal A breast cancer, which has a good prognosis.
Mutations in another gene, GATA3, also appeared to predict a good response to aromatase inhibitor therapy, while those in MALAT1, a long stretch of non-coding RNA, seemed to be associated with poor outcomes.
Mutations in most other significant genes occurred in frequencies too low to draw firm conclusions, but Ellis says it's premature to dismiss their importance.
“Breast cancer is so common that mutations that recur infrequently may still involve thousands of women,” Ellis says. “Only through further genomic studies will we be able to determine whether they also have a role in treatment response.”
At the recent American Society of Clinical Oncology meeting in Chicago, Ellis detailed a list of low-frequency mutations in estrogen-receptor-positive breast cancer that already can be targeted by existing drugs, many of which are approved for tumors other than those in the breast. He says that studies like this one may provide a backdrop for finding new cancer treatments based on a tumor's genomic signature rather than its location in the body.
“As a medical oncologist, I'm looking for clues for how to best treat my patients with breast cancer,” he says. “We're just beginning to see that many patients only have mutations that occur in low frequency. Targeting these mutations should be a focus of new clinical trials.”
Toward that goal, Ellis and Mardis will soon begin a new trial in patients with estrogen-receptor positive breast cancer, with treatment decisions based on the genomic signatures of tumors. Women likely to benefit from aromatase inhibitor therapy will receive it, but those unlikely to respond will be assigned to surgery followed by chemotherapy and drugs that target “driver” mutations in their tumors.
Ellis, MJ, Ding L, Shen D, Ley TJ, Piwnica-Worms D, Stuart JM, Wilson RK, Mardis ER. Whole-genome analysis informs breast caner response to aromatase inhibition. Nature. Advance online publication June 10, 2012.
The research is funded by the National Human Genome Research Institute, the National Cancer Institute, both at the National Institutes of Health (NIH), the Susan G. Komen for the Cure, the Fashion Footwear Charitable Foundation, Inc., and the Washington University Cancer Genome Initiative. Grant awards to the American College of Surgeons Oncology Group included NCI, the Breast Cancer Research Foundation, clinical trial support from Novartis and Pfizer and an NCI Center grant. The BRIGHT Institute is supported in part by an ATT/Emerson gift to the Siteman Cancer Center. The research is dedicated to the memory of Evelyn Lauder in recognition of her efforts to eradicate breast cancer.
Washington University School of Medicine's 2,100 employed and volunteer faculty physicians also are the medical staff of Barnes-Jewish and St. Louis Children's hospitals. The School of Medicine is one of the leading medical research, teaching and patient care institutions in the nation, currently ranked sixth in the nation by U.S. News & World Report. Through its affiliations with Barnes-Jewish and St. Louis Children's hospitals, the School of Medicine is linked to BJC HealthCare.
Media Contact
More Information:
http://www.wustl.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles

Bringing bio-inspired robots to life
Nebraska researcher Eric Markvicka gets NSF CAREER Award to pursue manufacture of novel materials for soft robotics and stretchable electronics. Engineers are increasingly eager to develop robots that mimic the…

Bella moths use poison to attract mates
Scientists are closer to finding out how. Pyrrolizidine alkaloids are as bitter and toxic as they are hard to pronounce. They’re produced by several different types of plants and are…
AI tool creates ‘synthetic’ images of cells
…for enhanced microscopy analysis. Observing individual cells through microscopes can reveal a range of important cell biological phenomena that frequently play a role in human diseases, but the process of…





















