Beyond the brain: vascular changes in the neck may play role in Alzheimer’s

The finding has potential implications for a better understanding of Alzheimer’s and other neurological disorders associated with aging.
The pilot study was published in the Journal of Alzheimer’s Disease Nov. 8 online ahead of print by researchers from the University at Buffalo, the University of Bradford in the United Kingdom and National Yang-Ming University School of Medicine in Taiwan. The authors caution that the study is small and that the results must be validated in larger, future studies.
They studied a hemodynamic abnormality in the internal jugular veins called jugular venous reflux or JVR. It occurs when the pressure gradient reverses the direction of blood flow in the veins, causing blood to leak backwards into the brain.
JVR occurs in certain physiological situations, if the internal jugular vein valves do not open and close properly, which occurs more frequently in the elderly. This reverse flow is also believed to impair cerebral venous drainage.
“We were especially interested to find an association between JVR and white matter changes in the brains of patients with Alzheimer’s disease and those with mild cognitive impairment,” says Robert Zivadinov, MD, PhD, FAAN, professor of neurology at the UB School of Medicine and Biomedical Sciences and senior author.
The brain’s white matter is made of myelin and axons that enable communication between nerve cells.
“Age-related white matter changes have long been associated with dementia and faster cognitive decline,” he says. “To the best of our knowledge, our study is the first to show that JVR is associated with a higher frequency of white matter changes, which occur in patients with mild cognitive impairment and Alzheimer’s disease.”
Ching-Ping Chung, the first author on the study and assistant professor of neurology at National Yang-Ming University, adds: “We are the first to observe that JVR may be associated with formation of these lesions in the brain, given the fact that Alzheimer’s patients have more white matter lesions than healthy people.
“If this observation is validated in larger studies,” she continues, “it could be significant for the development of new diagnostic tools and treatments for pathological white matter lesions developed in Alzheimer’s disease and other forms of dementia.”
White matter changes have been found to have a direct relationship to the buildup of amyloid plaque long seen as central to the development of Alzheimer’s disease.
“The accumulation of amyloid plaque may result from the inability of cerebrospinal fluid to be properly cleared from the brain,” says Clive Beggs, second author on the study and professor of medical engineering at the University of Bradford. In addition, he says, the study found that JVR appeared to be associated with dirty-appearing white matter, which is thought to represent early stage lesion formation.
“To the best of our knowledge, this is one of the first studies to explore the impact of dirty-appearing white matter in the elderly,” Beggs continues. He adds that the significance of dirty-appearing white matter in the elderly needs more study.
The research involved 12 patients with Alzheimer’s disease, 24 with mild cognitive impairment and 17 age-matched elderly controls. Participants underwent Doppler ultrasound exams and magnetic resonance imaging scans.
The impact of hemodynamic changes in veins from the brain to the neck has been the focus of numerous studies by Zivadinov and colleagues at UB and institutions worldwide.
“Given the major finding of our group in 2011 that both healthy controls and people with a variety of neurological diseases present with structural and hemodynamic changes of the extracranial venous system, we thought it was important to study how they might be involved in the development of Alzheimer’s disease and other important neurodegenerative conditions,” he explains.
Zivadinov notes that the frequency of JVR increases with aging and its accumulated effects on cerebral circulation may take many years to develop. Patients are likely to be asymptomatic for a long time, which would explain why the condition is seen in both healthy people and those with neurological diseases, he adds.
Co-authors besides Zivadinov, Chung and Beggs are Simon Shepherd of the Centre for Infection Control and Biophysics at the University of Bradford; Pei-Ning Wang, Chun-Yu Cheng and Han-Hwa Hu, all of Taipei Veterans General Hospital in Taipei and National Yang-Ming University; and Niels Bergsland, Deepa P. Ramasamy and Michael G. Dwyer all of the Buffalo Neuroimaging Analysis Center in the UB Department of Neurology.
Media Contact Information
Ellen Goldbaum
Senior Editor, Medicine
Tel: 716-645-4605
goldbaum@buffalo.edu
Twitter: @egoldbaum
Media Contact
More Information:
http://www.buffalo.eduAll latest news from the category: Health and Medicine
This subject area encompasses research and studies in the field of human medicine.
Among the wide-ranging list of topics covered here are anesthesiology, anatomy, surgery, human genetics, hygiene and environmental medicine, internal medicine, neurology, pharmacology, physiology, urology and dental medicine.
Newest articles
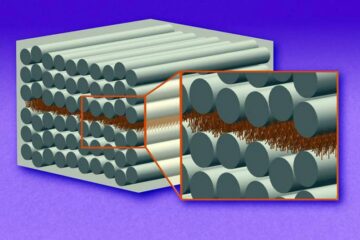
“Nanostitches” enable lighter and tougher composite materials
In research that may lead to next-generation airplanes and spacecraft, MIT engineers used carbon nanotubes to prevent cracking in multilayered composites. To save on fuel and reduce aircraft emissions, engineers…

Trash to treasure
Researchers turn metal waste into catalyst for hydrogen. Scientists have found a way to transform metal waste into a highly efficient catalyst to make hydrogen from water, a discovery that…
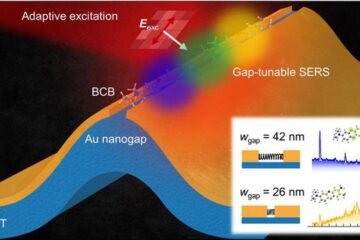
Real-time detection of infectious disease viruses
… by searching for molecular fingerprinting. A research team consisting of Professor Kyoung-Duck Park and Taeyoung Moon and Huitae Joo, PhD candidates, from the Department of Physics at Pohang University…





















