Higher volume reduces false positives in screening mammography

“Contrary to our expectations, we observed no clear association between volume and sensitivity,” said the study's lead author, Diana S.M. Buist, Ph.D., M.P.H., senior investigator at the Group Health Research Institute in Seattle. “We did, however, find that radiologists with higher interpretive volume had significantly lower false-positive rates and recalled fewer women per cancer detected.”
An exam result is considered to be a false positive when further testing is recommended for a suspicious lesion but no cancer is found. In addition to causing anxiety for patients, false positives prompt additional testing that costs approximately $1.6 billion per year, according to Dr. Buist.
The study, partially funded by the American Cancer Society and the National Cancer Institute, included a review of data from six Breast Cancer Surveillance Consortium mammography registries in California, North Carolina, New Hampshire, Vermont, Washington and New Mexico.
The researchers examined various measures of interpretive volume in relation to screening performance for 120 radiologists who interpreted 783,965 screening mammograms between 2002 and 2006. Volume was measured in four ways: the number of screening and diagnostic mammograms read by a radiologist annually—both separately and in combination—and the ratio of screening to total (diagnostic plus screening) mammograms. Screening performance was measured by sensitivity (the ability to detect all cancers present) and false-positive and cancer detection rates.
The results showed that performance varied not only by the number of exams interpreted, but also by the ratio of screening to total (diagnostic plus screening) mammograms.
“Our analysis demonstrated that screening interpretive performance is unlikely to be affected by volume alone, but rather by a balance in the interpreted exam composition,” Dr. Buist said. “The data suggest that radiologists who interpret screening mammograms should spend at least a portion of their time interpreting diagnostic mammograms, because radiologists who interpreted very few diagnostic mammograms had worse performance, even if they read a high volume of screening mammograms.”
Because the study found that radiologists with higher annual interpretive volumes had lower false-positive rates—while maintaining sensitivity rates similar to their lower-volume colleagues—the researchers simulated the effect of increasing the minimum interpretive volume required of radiologists practicing in the U.S., which is currently 960 mammograms every two years.
Based on 34 million women aged 40-79 receiving screening mammograms each year, the researchers estimated that increasing the annual minimum total volume requirement to 1,000 would result in 43,629 fewer women being recalled. The estimated cost associated with false-positive results would be reduced to $21.8 million.
“Recommending any increase in U.S. volume requirements would entail crucial decisions about the relative importance of cancer detection versus false positive exams and workforce issues, since changes could curtail workforce supply and women's mammography access,” Dr. Buist said.
“The Influence of Annual Interpretive Volume on Screening Mammography Performance in the United States.” Collaborating with Dr. Buist were Melissa L. Anderson, M.S., Sebastien J-P.A. Haneuse, Ph.D., Edward A. Sickles, M.D., Robert A. Smith, Ph.D., Patricia A. Carney, Ph.D., Stephen H. Taplin, M.D., M.P.H., Robert D. Rosenberg, M.D., Berta M. Geller, Ed.D., Tracy L. Onega, Ph.D., Barbara S. Monsees, M.D., Lawrence W. Bassett, M.D., Bonnie C. Yankaskas, Ph.D., Joann G. Elmore, M.D., M.P.H., Karla Kerlikowske, M.D., and Diana L. Miglioretti, Ph.D.
This study was supported by the American Cancer Society, the Longaberger Company's Horizon of Hope Campaign, Breast Cancer Stamp Fund, Agency for Healthcare Research and Quality, National Cancer Institute and National Cancer Institute Breast Cancer Surveillance Consortium.
Radiology is edited by Herbert Y. Kressel, M.D., Harvard Medical School, Boston, Mass., and owned and published by the Radiological Society of North America, Inc. (http://radiology.rsna.org/)
RSNA is an association of more than 46,000 radiologists, radiation oncologists, medical physicists and related scientists committed to excellence in patient care through education and research. The Society is based in Oak Brook, Ill. (RSNA.org)
For patient-friendly information on mammography, visit RadiologyInfo.org.
Media Contact
More Information:
http://www.rsna.orgAll latest news from the category: Medical Engineering
The development of medical equipment, products and technical procedures is characterized by high research and development costs in a variety of fields related to the study of human medicine.
innovations-report provides informative and stimulating reports and articles on topics ranging from imaging processes, cell and tissue techniques, optical techniques, implants, orthopedic aids, clinical and medical office equipment, dialysis systems and x-ray/radiation monitoring devices to endoscopy, ultrasound, surgical techniques, and dental materials.
Newest articles
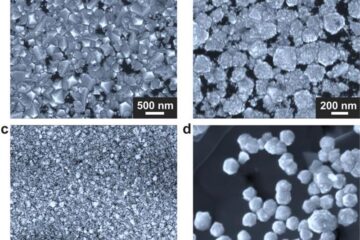
Making diamonds at ambient pressure
Scientists develop novel liquid metal alloy system to synthesize diamond under moderate conditions. Did you know that 99% of synthetic diamonds are currently produced using high-pressure and high-temperature (HPHT) methods?[2]…
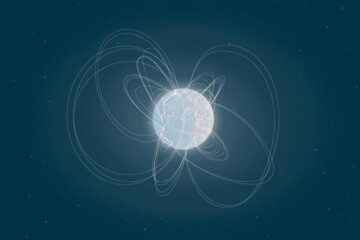
Eruption of mega-magnetic star lights up nearby galaxy
Thanks to ESA satellites, an international team including UNIGE researchers has detected a giant eruption coming from a magnetar, an extremely magnetic neutron star. While ESA’s satellite INTEGRAL was observing…
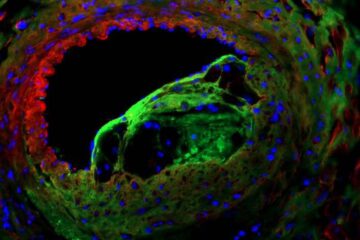
Solving the riddle of the sphingolipids in coronary artery disease
Weill Cornell Medicine investigators have uncovered a way to unleash in blood vessels the protective effects of a type of fat-related molecule known as a sphingolipid, suggesting a promising new…





















