Soothing Cells, Peaceful Protein Could Hold Promise for Treating Autoimmune Uveitis
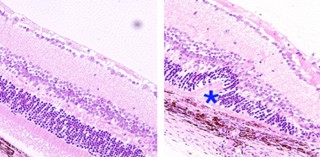
A healthy mouse retina (left) and distinctive folds in a mouse retina damaged by autoimmune uveitis (right). Wang et al. Nature Medicine, April 2014
Uveitis occurs when immune cells invade the eye, causing inflammation and swelling. The NEI researchers found a unique immune cell population that suppresses eye inflammation and reduces the severity of uveitis by releasing a protein called interleukin-35 (IL-35). The discovery, published in Nature Medicine, could lead to the development of new drugs based on IL-35 and to cellular therapies for uveitis.
Corticosteroids and other drugs that have a general suppressing effect on the immune system are typically the first-line treatments for uveitis. But over time, these drugs can cause a number of side effects, including weight gain, stomach ulcers, diabetes, heart disease, cataract and glaucoma.
Biologics, which are drugs that are designed to target specific biological processes in the body, are another option. But currently available biologics were developed for a variety of diseases other than uveitis, and relatively little is known about the long-term benefits and risks of using them against uveitis.
“Usually, physicians use steroids and other current treatments sparingly, in order to avoid complications,” said Charles Egwuagu, Ph.D., M.P.H., who is chief of the Molecular Immunology section in NEI’s Laboratory of Immunology. “There has been a big push to develop biologics that would be more specific and effective for uveitis.”
Uveitis literally means inflammation of the uvea, which is a middle layer of the eye that includes the iris (the colored ring) and the choroid, a tissue filled with tiny blood vessels. Normally, blood flow within these vessels is tightly regulated, creating a barrier between the bloodstream and the delicate tissues of the eye. But in uveitis, immune cells in the blood creep out of the vessels and wreak havoc in the eye. They can damage not only the uvea, but also the retina and the optic nerve. (The retina is the light-sensitive tissue at the back of the eye, and the optic nerve connects the retina to the brain.)
Uveitis can be triggered by eye infections or by autoimmunity, a process in which an overly aggressive response by the immune system results in damage to the body’s own tissues. Autoimmune uveitis may occur as part of other autoimmune diseases such as juvenile rheumatoid arthritis, multiple sclerosis, Behçet’s disease, and systemic lupus erythematosus. It is estimated that autoimmune uveitis accounts for 10 percent of all visual disabilities in the United States.
Dr. Egwuagu and his team have been working to understand autoimmune uveitis and other such disorders by studying complex feedback loops that are built into the immune response and normally keep it from turning against the body. Among immune cells, T cells generally serve as mobile infantry units, attacking invaders at close range. Meanwhile, B cells serve as the artillery units, attacking with guided missiles known as antibodies. In smaller numbers, there are also regulatory T cells and B cells that act as peacemakers, quieting down their armed, hostile counterparts. In recent years, there has been growing interest in harnessing these regulatory immune cells to calm down autoimmune responses.
There has been particular interest in IL-35, a member of a family of proteins called cytokines, which help tune immune responses. IL-35 was first discovered in 2007. It is produced by regulatory T cells and acts as a “calm down” signal for other cells. It is actually a pair of separate smaller proteins intimately joined together, and has proven difficult to purify or manufacture. Dr. Egwuagu’s group is one of only two labs in the country that have been able to produce and study the complete protein, without using extra bits of protein called linkers to connect its two parts.
The researchers tested whether or not IL-35 could suppress autoimmune uveitis in a mouse model. To induce autoimmune uveitis in mice, they gave the mice injections of a retinal protein that appears to agitate immune cells in people with the condition. These mice developed damage to the uvea, retina, and optic nerve. But IL-35 injections given on the same day of disease induction helped prevent uveitis. When given up to 10 days after disease induction, IL-35 suppressed uveitis.
In other experiments done on laboratory-grown mouse cells, the researchers found that IL-35 protects against uveitis by changing the destiny of primitive B cells. Without IL-35, those cells typically become antibody-producing B cells. But IL-35 turns a fraction of those cells into regulatory B cells that produce more IL-35, creating a chain reaction of calm. The researchers found that IL-35 has the same effect on human B cells grown in the lab, suggesting it could have similar therapeutic effects in people as in mice.
Finally, the researchers found that they could reverse uveitis in mice with injections of the regulatory B cells that produce IL-35, instead of injecting the protein itself. Ultimately, using the cells as therapy may be better than using the protein, Dr. Egwuagu said.
“We suspect that IL-35 is likely to have unpredictable side effects,” he said. But the B cells responsible for producing it may produce other substances that balance these effects. “If you can grow and select for these cells, you can probably calibrate the effects of IL-35,” he said.
Much work remains to be done to see if people with autoimmune uveitis could benefit from IL-35 or the cells that produce it. Testing in other animal models and methods for ramping up production of IL-35 will be necessary. Dr. Egwuagu also plans to investigate whether some people with autoimmune uveitis have a reduction or defect in regulatory B cells. If so, they would likely benefit from treatment with IL-35 or the regulatory B cells that produce it, said Dr. Egwuagu. There is also interest among the broader research community in determining if these therapies might be useful against other autoimmune diseases or organ transplant rejection.
Reference: Wang RX et al. “Interleukin-35 induces regulatory B cells that suppress autoimmune disease.” Nature Medicine, April 2014. DOI: 10.1038/nm.3554.
###
NEI leads the federal government's research on the visual system and eye diseases. NEI supports basic and clinical science programs that result in the development of sight-saving treatments. For more information, visit http://www.nei.nih.gov.
Media Contact
All latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles

Superradiant atoms could push the boundaries of how precisely time can be measured
Superradiant atoms can help us measure time more precisely than ever. In a new study, researchers from the University of Copenhagen present a new method for measuring the time interval,…

Ion thermoelectric conversion devices for near room temperature
The electrode sheet of the thermoelectric device consists of ionic hydrogel, which is sandwiched between the electrodes to form, and the Prussian blue on the electrode undergoes a redox reaction…

Zap Energy achieves 37-million-degree temperatures in a compact device
New publication reports record electron temperatures for a small-scale, sheared-flow-stabilized Z-pinch fusion device. In the nine decades since humans first produced fusion reactions, only a few fusion technologies have demonstrated…





















