Major genetic study identifies clearest link yet to obesity risk

Obesity is a major cause of disease, associated with an increased risk of type 2 diabetes, heart disease and cancer. It is typically measured using body mass index (BMI). As a result of reduced physical activity and increased food consumption, the prevalence of obesity is increasing worldwide. According to the 2001 Health Survey for England, over a fifth of males and a similar proportion of females aged 16 and over in England were classified as obese. Half of men and a third of women were classified as overweight.
Scientists from the Peninsula Medical School, Exeter, and the University of Oxford first identified a genetic link to obesity through a genome-wide study of 2,000 people with type 2 diabetes and 3,000 controls. This study was part of the Wellcome Trust Case Control Consortium, one of the biggest projects ever undertaken to identify the genetic variations that may predispose people to or protect them from major diseases. Through this genome-wide study, the researchers identified a strong association between an increase in BMI and a variation, or “allele”, of the gene FTO. Their findings are published online today in the journal Science.
The researchers then tested a further 37,000 samples for this gene from Bristol, Dundee and Exeter as well as a number of other regions in the UK and Finland.
The study found that people carrying one copy of the FTO allele have a 30% increased risk of being obese compared to a person with no copies. However, a person carrying two copies of the allele has a 70% increased risk of being obese, being on average 3kg heavier than a similar person with no copies. Amongst white Europeans, approximately one in six people carry both copies of the allele.
“As a nation, we are eating more but doing less exercise, and so the average weight is increasing, but within the population some people seem to put on more weight than others,” explains Professor Andrew Hattersley from the Peninsula Medical School. “Our findings suggest a possible answer to someone who might ask 'I eat the same and do as much exercise as my friend next door, so why am I fatter?' There is clearly a component to obesity that is genetic.”
The researchers currently do not know why people with copies of the FTO allele have an increased BMI and rates of obesity.
“Even though we have yet to fully understand the role played by the FTO gene in obesity, our findings are a source of great excitement,” says Professor Mark McCarthy from the University of Oxford. “By identifying this genetic link, it should be possible to improve our understanding of why some people are more obese, with all the associated implications such as increased risk of diabetes and heart disease. New scientific insights will hopefully pave the way for us to explore novel ways of treating this condition.”
The findings were welcomed by Dr Mark Walport, Director of the Wellcome Trust.
“This is an exciting piece of work that illustrates why it was so important to sequence the human genome,” says Dr Walport. “Obesity is one of the most challenging problems for public health in the UK. The discovery of a gene that influences the development of obesity in the general population provides a new tool for understanding how some people appear to gain weight more easily than others. This discovery, along with further results expected from the Wellcome Trust Case Control Consortium later this year, will open up a wealth of new avenues to understand and treat common diseases.”
The FTO gene was first discovered whilst studying the DNA of a cohort of patients with type 2 diabetes. The risk of developing type 2 diabetes increases significantly for obese people. Through its effect on BMI, having one copy of the FTO allele increases the risk of developing type 2 diabetes by 25%, having two by 50%.
“We welcome this result, which holds promise for tackling rising levels of obesity and the associated risk of developing type 2 diabetes,” says Professor Simon Howell, Chair of Diabetes UK, which funded the original collection of samples from people with diabetes. “The discovery has been possible not only because of exemplary team work of scientists from a large number of institutions but also because of the cooperation of the 5,000 diabetes patients and 37,000 people without diabetes who gave blood samples for the study.”
Media Contact
More Information:
http://www.wellcome.ac.ukAll latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles

Bringing bio-inspired robots to life
Nebraska researcher Eric Markvicka gets NSF CAREER Award to pursue manufacture of novel materials for soft robotics and stretchable electronics. Engineers are increasingly eager to develop robots that mimic the…

Bella moths use poison to attract mates
Scientists are closer to finding out how. Pyrrolizidine alkaloids are as bitter and toxic as they are hard to pronounce. They’re produced by several different types of plants and are…
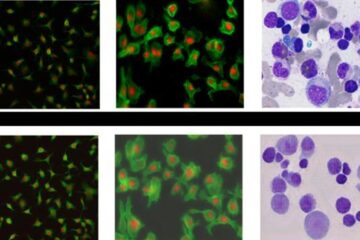
AI tool creates ‘synthetic’ images of cells
…for enhanced microscopy analysis. Observing individual cells through microscopes can reveal a range of important cell biological phenomena that frequently play a role in human diseases, but the process of…





















