Science researchers genetically transform immune cells into tumor fighters

A team of researchers has genetically engineered normal immune cells to become specialized tumor fighters, demonstrating for the first time that these engineered cells can persist in the body and shrink large tumors in humans.
Two of the 17 people with advanced melanoma who received the experimental treatment saw their tumors shrink and were declared clinically free of disease more than a year and half after the therapy began, Steven A. Rosenberg of the National Cancer Institute and his colleagues report in a study published online by the journal Science at the Science Express website on 31 August. Science and Science Express are published by AAAS, the nonprofit science society.
So far, the therapy has only been used in this small group of melanoma patients, but Rosenberg says his team has demonstrated ways to engineer similar immune cells in the laboratory that would attack more common tumors such as breast, lung and liver cancers.
The technique developed by the Science researchers “represents the first time that gene manipulations have been shown to cause tumor regression in humans,” Rosenberg says.
“This work marks an important next step in harnessing the power of our immune systems to fight cancer. The publication of this paper should help highlight the significant work to a broad spectrum of people, including patients, clinicians and those involved in basic research,” said Stephen Simpson, Science's senior editor, immunology.
Rosenberg and colleagues have a long history of looking for ways to boost the body's natural immune defenses against cancer, focusing specifically on T cells, a special type of immune cell that can recognize and attack “foreign” cells such as those found in tumors. In their earlier experiments, the researchers removed tumor-fighting T cells from melanoma patients and multiplied these cells in the laboratory. After using chemotherapy to clear out a patient's old T cells, the researchers repopulated the patients' immune systems with these new fighters.
But some people with melanoma don't have these tumor-fighting T cells, and in other types of cancer it's difficult to identify T cells that attack tumors, Rosenberg says, so the researchers had to come up with a way to create these types of T cells from scratch.
T cells carry a receptor protein on their surface that recognizes specific molecules called antigens on tumor cells. The receptor's genetic makeup determines the antigen types that the T cell can recognize, so that some cells contain genes that make a T cell receptor that homes in on melanoma cells, while other cells contain genes that make a T cell receptor that recognizes breast or lung cancer cells.
With this in mind, Rosenberg and colleagues created tumor fighters by removing normal T cells from people with advanced metastatic melanoma, genetically engineering these normal cells to carry the receptor that recognizes melanoma cells and returning these “re-armed” cells to rebuild the patients' immune systems.
“We can take normal lymphocytes from patients and convert them to tumor-reactive cells,” Rosenberg says, adding that the engineered cells could be tailored to fight tumors other than melanoma. “We've identified T cell receptors that will now recognize common cancers,” he notes.
The newly engineered T cells showed signs of persistence in 15 of the patients in the study, making up at least 10 percent of their circulating T cells for at least two months after treatment. New T cell levels were higher in the two people whose tumors shrunk noticeably with the treatment.
Rosenberg and colleagues are now searching for ways to fine-tune the treatment so that greater numbers of the engineered T cells will survive and continue expressing their new receptor genes, since their expression does seem to wane over time, the Science researchers found.
Devising new ways to insert the receptor genes in the T cells, usually encoded in a retrovirus, has been one of the most challenging aspects of the treatment, Rosenberg says. “It's a lot of sophisticated molecular biology and most of our work is going into designing retroviruses, putting genes into cells efficiently and getting them expressed.”
Media Contact
More Information:
http://www.aaas.orgAll latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles
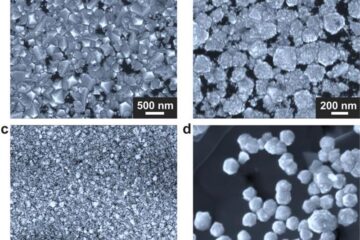
Making diamonds at ambient pressure
Scientists develop novel liquid metal alloy system to synthesize diamond under moderate conditions. Did you know that 99% of synthetic diamonds are currently produced using high-pressure and high-temperature (HPHT) methods?[2]…
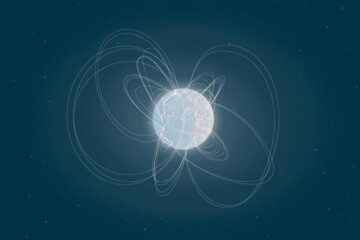
Eruption of mega-magnetic star lights up nearby galaxy
Thanks to ESA satellites, an international team including UNIGE researchers has detected a giant eruption coming from a magnetar, an extremely magnetic neutron star. While ESA’s satellite INTEGRAL was observing…
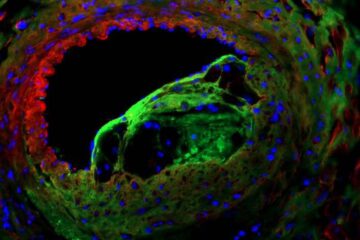
Solving the riddle of the sphingolipids in coronary artery disease
Weill Cornell Medicine investigators have uncovered a way to unleash in blood vessels the protective effects of a type of fat-related molecule known as a sphingolipid, suggesting a promising new…





















