Stem cell transplants improve recovery in animal models for stroke, cerebral palsy

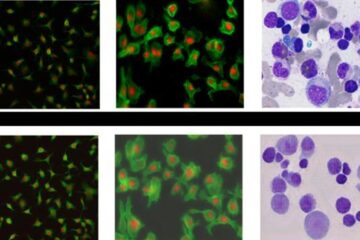
Using a commonly utilized animal model for stroke, researchers administered a dose of 200,000-400,000 human stem cells into the brain of animals that had experienced significant loss of mobility and other functions. The stem cells used in the study were a recently discovered stem cell type, referred to as multipotent adult progenitor cells, or MAPCs.
Treated animals experienced at least 25 percent greater improvement in motor and neurological performance than controls, said Dr. Cesario V. Borlongan, neuroscientist at the Medical College of Georgia and the Veterans Affairs Medical Center in Augusta.
The findings are being presented April 7 during the 58th annual meeting of the American Academy of Neurology in San Diego.
In humans, the findings hopefully will translate to incremental but important recovery advances, said Dr. David Hess, adult stroke specialist, chair of the MCG Department of Neurology and a study co-author. “The single largest cause of disability among adults in ths U.S. is stroke,” said Dr. Hess. “It’s a huge public health problem in the world.” He hopes one day stem cell therapy, along with aggressive physical therapy and possibly tPA can work synergistically to reduce that disability.
“These are not going to be cures, but this level of recovery is significant, and could help get somebody out of a bed and into a wheelchair or out of a wheelchair to walking with a cane or from a cane to walking unassisted. If somebody can go from a wheelchair to a cane that is a big improvement, that is how we look at it,” Dr. Hess said.
Adult animals were tested across a range of standardized tasks both before and after undergoing the surgically induced stroke, and measurements were made of their performance. Following the stroke, both control animals and those that received a single injection of stem cells were evaluated for a period of up to 2 months. Improvements in stem cell treated animals included enhanced performance across the range of tests, which examined strength, balance, agility and fine motor skills, and also included greater recovery of injured tissue.
“A single dose of the cells produce robust behavioral recovery at an early period post-transplantation and the recovery was durable, lasting up to two months, which was the entire length of this study,” Dr. Borlongan said. “Furthermore, animals continued to show improvement over time.” In the newborn model of ischemic injury, enhanced recovery was found within two weeks.
Even though less than 1 percent of the transplanted cells were present two months later, animals receiving treatment developed new neurons, apparently formed from endogenous stem cells. “The mechanism that we are putting forward is these donor cells are secreting nourishing trophic factors that are helping the host brain cells survive and stimulating stem cells from the host to multiply,” Dr. Borlongan said.
To help mimic potential clinical scenarios for stroke victims, transplants were performed seven days after the initial injury. Currently, ischemic stroke patients may be treated with tPA, the only FDA-approved stroke treatment available, but must receive treatment within three hours from the time the stroke initially occurs. As a result, 95-97 percent of ischemic stroke victims never receive treatment with tPA.
In the adult stroke model, MCG researchers found giving stem cells increased the number of injured cells that survived in the area just outside the area of greatest damage, also referred to as the ischemic core, by 5-20 percent.
“Up to this point, all the treatment approaches, including transplantation and tPA, cannot get rid of that ischemic core,” Dr. Borlongan said. “But outside of that core there is a lining, what we call the penumbra, and that penumbra, if you do not treat it over time, becomes part of the core. We are showing, that even one week after a stroke, we are able to increase the number of cells surviving along that penumbra and that is how we feel it is producing significant recovery, by rescuing cells within the penumbra.”
Animals in the model of cerebral palsy, a condition caused by an ischemic injury similar to stroke but occurring before or during birth, also experienced at least a 25 percent improvement over controls. Rodent stem cells were used in this model, a larger percent of donated cells survived and within two weeks matured into neurons in the young, more pliable brains, Dr. Borlongan said. Also, close donor matching seemed unnecessary. Unmatched transplants, from the same species, and gentically identical transplants yielded essentially equal results.
Athersys, Inc., a Cleveland-based biopharmaceutical company pursuing cell therapy programs in cardiovascular disease, stroke, cancer and other diseases, funded the research in which previously frozen human or rodent multipotent adult progenitor cells, which the company calls MultiStem™, were thawed and injected directly into the brain.
Researchers believe that MultiStem™ cells are able to deliver a therapeutic benefit in multiple ways, for example by producing factors that limit tissue damage and stimulate repair, according to Dr. Gil Van Bokkelen, the company’s chairman and chief executive officer. In addition, MultiStem™ cells can safely mature into a broad range of cell types and can be produced on a large scale, something which should ease the move toward clinical studies and eventual clinical use. “Given the number of stroke victims each year, it would be a big step forward if a safe and effective stem cell therapy could be produced, conveniently stored, and efficiently delivered on a widespread basis. We believe that we can achieve that with MultiStem™,” commented Dr. Van Bokkelen.
In extensive animal testing, the mature stem cells have been shown to be safe, and do not form tumors or other abnormal tissue, a potential problem seen with embryonic stem cells. Furthermore, MultiStem™ cells generally do not require the close genetic matching between donor and recipient that is needed for a bone marrow or conventional stem cell transplant, according to company executives.
Another advantage is that use of immunosuppressive drugs does not appear to be required, in contrast to other types of stem cell treatment. Animals that received MultiStem™ without immunosuppression of any kind did just as well as animals that received MultiStem™ treatment along with daily doses of Cyclosporine A, a drug typically given to transplant recipients to prevent rejection. Such drugs can cause undesired side effects, and may be problematic if administered to patients for long periods of time. These results are consistent with those seen in other models, such as using MultiStem™ to treat damage caused by heart attacks, company officials say.
Although they have not specifically looked at whether stem cell therapy might be useful months after an ischemic event, MCG researchers and company scientists believe early therapy likely will be the most successful.
The researchers already are working with the Food and Drug Administration with the goal of beginning clinical trials within the next few years.
In preparation for potential clinical use, the researchers are pursuing transplants in larger animal models and studying how MultiStem™ cells work in living human brain tissue housed at the MCG Human Brain Bank, directed by Dr. Sergei Kirov.
“Number one is safety,” said Dr. Borlongan. “We are moving more aggressively into carrying this into the clinic but, at the same time, we are going to be very cautious and thorough in monitoring for any safety issues.”
Researchers also are working toward delivering the stem cells intravenously, an approach they believe will work because the cells naturally migrate to an injury site.
Other co-authors include Dr. James E. Carroll, chief of the Section of Pediatric Neurology; Dr. Lin Xu, MCG research scientist; Drs. Noriyuki Matsaukawa, Guolong Yu, Takao Yasuhara and Koichi Hara, MCG postdoctoral fellows; and Athersys scientists Robert W. Mays, and Robert J. Deans.
Media Contact
More Information:
http://www.mcg.eduAll latest news from the category: Life Sciences and Chemistry
Articles and reports from the Life Sciences and chemistry area deal with applied and basic research into modern biology, chemistry and human medicine.
Valuable information can be found on a range of life sciences fields including bacteriology, biochemistry, bionics, bioinformatics, biophysics, biotechnology, genetics, geobotany, human biology, marine biology, microbiology, molecular biology, cellular biology, zoology, bioinorganic chemistry, microchemistry and environmental chemistry.
Newest articles

Bringing bio-inspired robots to life
Nebraska researcher Eric Markvicka gets NSF CAREER Award to pursue manufacture of novel materials for soft robotics and stretchable electronics. Engineers are increasingly eager to develop robots that mimic the…

Bella moths use poison to attract mates
Scientists are closer to finding out how. Pyrrolizidine alkaloids are as bitter and toxic as they are hard to pronounce. They’re produced by several different types of plants and are…
AI tool creates ‘synthetic’ images of cells
…for enhanced microscopy analysis. Observing individual cells through microscopes can reveal a range of important cell biological phenomena that frequently play a role in human diseases, but the process of…





















